Flumazenil
Flumazenil (also known as flumazepil, code name Ro 15-1788) is a selective GABAA receptor antagonist[1] administered via injection, otic insertion, or intranasally. Therapeutically, it acts as both an antagonist and antidote to benzodiazepines (particularly in cases of overdose), through competitive inhibition.
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Anexate, Lanexat, Mazicon, Romazicon |
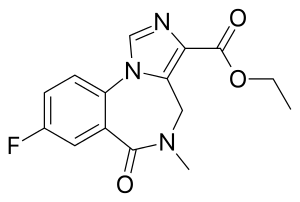
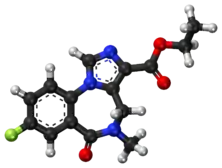
| Other names | ethyl 8-fluoro- 5,6-dihydro- 5-methyl- 6-oxo- 4H- imidazo [1,5-a] [1,4] benzodiazepine- 3-carboxylate |
| AHFS/Drugs.com | Monograph |
| Pregnancy category |
|
| Routes of administration | IV |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Metabolism | Hepatic |
| Elimination half-life | 7-15 min (initial) 20-30 min (brain) 40-80 min (terminal) |
| Excretion | Urine 90-95% Feces 5-10% |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.128.069 |
| Chemical and physical data | |
| Formula | C15H14FN3O3 |
| Molar mass | 303.293 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
It was first characterized in 1981,[2] and was first marketed in 1987 by Hoffmann-La Roche under the trade name Anexate. However, it did not receive FDA approval until December 20, 1991. The developer lost its exclusive patent rights in 2008; so at present, generic formulations of this drug are available. Intravenous flumazenil is primarily used to treat benzodiazepine overdoses and to help reverse anesthesia. Administration of flumazenil by sublingual lozenge and topical cream has also been tested.[3][4]
Medical uses
Flumazenil benefits patients who become excessively drowsy after use of benzodiazepines for either diagnostic or therapeutic procedures.[5]
The drug has been used as an antidote in the treatment of benzodiazepine overdoses.[5] It reverses the effects of benzodiazepines by competitive inhibition at the benzodiazepine (BZ) recognition site on the GABA/benzodiazepine receptor complex. There are many complications that must be taken into consideration when used in the acute care setting.[5] These include lowered seizure threshold, agitation, and anxiousness. Flumazenil's short half-life requires multiple doses. Because of the potential risks of withdrawal symptoms and the drug's short half-life, patients must be carefully monitorered to prevent recurrence of overdose symptoms or adverse side effects.
Flumazenil is also sometimes used after surgery to reverse the sedative effects of benzodiazepines. This is similar to naloxone's application to reverse the effect of opiates and opioids following surgery. Administration of the drug requires careful monitoring by an anesthesiologist due to potential side effects and serious risks associated with over-administeration. Likewise, post-surgical monitoring is also necessary because flumazenil can mask the apparent metabolization ("wearing off") of the drug after removal of patient life-support and monitoring equipment.
Flumazenil has been effectively used to treat overdoses of non-benzodiazepine hypnotics, such as zolpidem, zaleplon and zopiclone (also known as "Z-drugs").[6]
It may also be effective in reducing excessive daytime sleepiness while improving vigilance in primary hypersomnias, such as idiopathic hypersomnia.[7]
The drug has also been used in hepatic encephalopathy. It may have beneficial short‐term effects in people with cirrhosis, but there is no evidence for long-term benefits.[8]
The onset of action is rapid, and effects are usually seen within one to two minutes. The peak effect is seen at six to ten minutes. The recommended dose for adults is 200 μg every 1–2 minutes until the effect is seen, up to a maximum of 3 mg per hour. It is available as a clear, colourless solution for intravenous injection, containing 500 μg in 5 mL.
Many benzodiazepines (including midazolam) have longer half-lives than flumazenil. Therefore, in cases of overdose, repeat doses of flumazenil may be required to prevent recurrent symptoms once the initial dose of flumazenil wears off.
It is hepatically metabolised to inactive compounds which are excreted in the urine. Individuals who are physically dependent on benzodiazepines may suffer benzodiazepine withdrawal symptoms, including seizure, upon rapid administration of flumazenil.
It is not recommended for routine use in those with a decreased level of consciousness.[9]
In terms of drug enforcement initiatives, diversion control programs and required post-marketing surveillance of adverse events, orders for flumazenil may trigger a prescription audit to the search for benzodiazepine misuse and for clinically significant adverse reactions related to their use.[10]
PET radioligand
Radiolabeled with the radioactive isotope carbon-11, flumazenil may be used as a radioligand in neuroimaging with positron emission tomography to visualize the distribution of GABAA receptors in the human brain.[11]
Treatment for benzodiazepine dependence & tolerance
In Italy, the gold standard for treatment of high-dose benzodiazepine dependency is 8–10 days of low-dose, slowly infused flumazenil.[12] One addiction treatment centre in Italy has used flumazenil to treat over 300 patients who were dependent on high doses of benzodiazepines (up to 70 times higher than conventionally prescribed) with physicians being among the clinic's most common patients.[13]
Epileptic patients who have become tolerant to the anti-seizure effects of the benzodiazepine clonazepam became seizure-free for several days after treatment with 1.5 mg of flumazenil.[14] Similarly, patients who were dependent on high doses of benzodiazepines (median dosage 333 mg diazepam-equivalent) were able to be stabilised on a low dose of clonazepam after 7–8 days of treatment with flumazenil.[15]
Flumazenil has been tested against placebo in benzo-dependent subjects. Results showed that typical benzodiazepine withdrawal effects were reversed with few to no symptoms.[16] Flumazenil was also shown to produce significantly fewer withdrawal symptoms than saline in a randomized, placebo-controlled study with benzodiazepine-dependent subjects. Additionally, relapse rates were much lower during subsequent follow-up.[17]
In vitro studies of tissue cultured cell lines have shown that chronic treatment with flumazenil enhanced the benzodiazepine binding site where such receptors have become more numerous and uncoupling/down-regulation of GABAA has been reversed.[18][19][20] After long-term exposure to benzodiazepines, GABAA receptors become down-regulated and uncoupled. Growth of new receptors and recoupling after prolonged flumazenil exposure has also been observed. It is thought this may be due to increased synthesis of receptor proteins.[21]
Flumazenil was found to be more effective than placebo in reducing feelings of hostility and aggression in patients who had been free of benzodiazepines for 4–266 weeks.[22] This may suggest a role for flumazenil in treating protracted benzodiazepine withdrawal symptoms.
Low-dose, slow subcutaneous flumazenil administration is a safe procedure for patients withdrawing from long-term, high-dose benzodiazepine dependency.[23] It has a low risk of seizures even amongst those who have experienced convulsions when previously attempting benzodiazepine withdrawal.[24]
Clinical pharmacology
Flumazenil, an imidazobenzodiazepine derivative, antagonizes the actions of benzodiazepines on the central nervous system. Flumazenil competitively inhibits the activity at the benzodiazepine recognition site on the GABA/benzodiazepine receptor complex.[25] It also exhibits weak partial agonism of GABAA receptor complexes that contain α6-type monomers; the clinical relevance of this is unknown.[26]
Flumazenil does not antagonize all of the central nervous system effects of drugs affecting GABA-ergic neurons by means other than the benzodiazepine receptor (including ethanol, barbiturates, and most anesthetics) and does not reverse the effects of opioids. It will however antagonize the action of non-benzodiazepine z-drugs, such as zolpidem and zopiclone, because they act via the benzodiazepine site of the GABA receptor[27] - it has been used to successfully treat z-drug overdose.[27][28][29]
Pharmacodynamics
Intravenous flumazenil has been shown to antagonize sedation, impairment of recall, psychomotor impairment and ventilatory depression produced by benzodiazepines in healthy human volunteers.
The duration and degree of reversal of sedative benzodiazepine effects are related to the dose and plasma concentrations of flumazenil.
Availability
Flumazenil is sold under a wide variety of brand names worldwide like Anexate, Lanexat, Mazicon, Romazicon. In India it is manufactured by Roche Bangladesh Pharmaceuticals and USAN Pharmaceuticals.
See also
References
- Whitwam, J. G.; Amrein, R. (1995-01-01). "Pharmacology of flumazenil". Acta Anaesthesiologica Scandinavica. Supplementum. 108: 3–14. doi:10.1111/j.1399-6576.1995.tb04374.x. ISSN 0515-2720. PMID 8693922. S2CID 24494744.
- Whitwam, James. G. (1988). "Flumazenil: a benzodiazepine antagonist". BMJ. 297 (6655): 999–1000. doi:10.1136/bmj.297.6655.999. PMC 1834756. PMID 2903780.
- D.B. Rye; D.L. Bliwise; K. Parker; L.M. Trotti; P. Saini; J. Fairley; A. Freeman; P.S. Garcia; M.J. Owens; J.C. Ritchie; A. Jenkins (21 November 2012). "Modulation of Vigilance in the Primary Hypersomnias by Endogenous Enhancement of GABAA Receptors". Sci. Transl. Med. 4 (161): 161ra151. doi:10.1126/scitranslmed.3004685. PMID 23175709. S2CID 44236050.
- http://clinicaltrials.gov/show/NCT01183312
- Goldfrank, Lewis R. (2002). Goldfrank's toxicologic emergencies. New York: McGraw-Hill Medical Publ. Division. ISBN 978-0-07-136001-2.
- Nelson, Lewis H.; Flomenbaum, Neal; Goldfrank, Lewis R.; Hoffman, Robert Louis; Howland, Mary Deems; Neal A. Lewin (2006). Goldfrank's toxicologic emergencies. New York: McGraw-Hill, Medical Pub. Division. ISBN 978-0-07-147914-1.
- D.B. Rye; D.L. Bliwise; K. Parker; L.M. Trotti; P. Saini; J. Fairley; A. Freeman; P.S. Garcia; M.J. Owens; J.C. Ritchie; A. Jenkins (2012). "Modulation of Vigilance in the Primary Hypersomnias by Endogenous Enhancement of GABAA Receptors". Sci. Transl. Med. 4 (161): 161ra151. doi:10.1126/scitranslmed.3004685. PMID 23175709. S2CID 44236050.
- Goh, ET; Andersen, ML; Morgan, MY; Gluud, LL (10 August 2017). "Flumazenil versus placebo or no intervention for people with cirrhosis and hepatic encephalopathy" (PDF). Cochrane Database of Systematic Reviews. 8: CD002798. doi:10.1002/14651858.CD002798.pub4. PMC 6483298. PMID 28796283.
- Wood, Lawrence D. H.; Hall, Jesse B.; Schmidt, Gregory D. 1952 (2005). Principles of critical care. McGraw-Hill Professional. ISBN 978-0-07-141640-5.
- Kawano DF, Ueta J, Sankarankutty AK, Pereira LR, de Freitas O (2009). "Midazolam-related drug interactions: detection of risk situations to the patient safety in a brazilian teaching hospital". J Patient Saf. 5 (2): 69–74. doi:10.1097/PTS.0b013e3181a5dafa. PMID 19920444. S2CID 12973546.
- Alexander Hammers; Matthias J. Koepp; Mark P. Richardson; Rene Hurlemann; David J. Brooks & John S. Duncan (June 2003). "Grey and white matter flumazenil binding in neocortical epilepsy with normal MRI. A PET study of 44 patients". Brain. 126 (Pt 6): 1300–1308. doi:10.1093/brain/awg138. PMID 12764053.
- Lugoboni, Fabio; Faccini, Marco; Quaglio, Gianluca; Casari, Rebecca; Albiero, Anna; Pajusco, Benedetta (2011). "Agonist substitution for high-dose benzodiazepine-dependent patients: let us not forget the importance of flumazenil". Addiction. 106 (4): 853. doi:10.1111/j.1360-0443.2010.03327.x. ISSN 0965-2140. PMID 21320225.
- Lugoboni, Fabio; Leone, Roberto (2012). "What is Stopping Us from Using Flumazenil?". Addiction. 107 (7): 1359. doi:10.1111/j.1360-0443.2012.03851.x. ISSN 0965-2140. PMID 22509854.
- Savic, I (1991). "Feasibility of reversing benzodiazepine tolerance with flumazenil". The Lancet. 337 (8734): 133–137. doi:10.1016/0140-6736(91)90799-U. ISSN 0140-6736. PMID 1670787. S2CID 41180892.
- Quaglio, Gianluca; Pattaro, Cristian; Gerra, Gilberto; Mathewson, Sophie; Verbanck, Paul; Des Jarlais, Don C.; Lugoboni, Fabio (2012). "High dose benzodiazepine dependence: Description of 29 patients treated with flumazenil infusion and stabilised with clonazepam". Psychiatry Research. 198 (3): 457–462. doi:10.1016/j.psychres.2012.02.008. ISSN 0165-1781. PMID 22424905. S2CID 28979824.
- G. Gerra; G. Giucasto; A. Zaimovic; G. Fertonani; B. Chittolini; P. Avanzini; R. Caccavari & R. Delsignore (June 1996). "Intravenous flumazenil following prolonged exposure to lormetazepam in humans: lack of precipitated withdrawal". International Clinical Psychopharmacology. 11 (2): 81–88. doi:10.1097/00004850-199611020-00002. PMID 8803645.
- Gerra, G.; Zaimovic, A.; Giusti, F.; Moi, G.; Brewer, C. (2002). "Intravenous flumazenil versus oxazepam tapering in the treatment of benzodiazepine withdrawal: a randomized, placebo-controlled study". Addiction Biology. 7 (4): 385–395. doi:10.1080/1355621021000005973. ISSN 1355-6215. PMID 14578014. S2CID 21255719.
- Danka Pericic; Josipa Lazic & Dubravka Svob Strac (August 2005). "Chronic treatment with flumazenil enhances binding sites for convulsants at recombinant alpha(1)beta(2)gamma(2S) GABA(A) receptors". Biomedicine & Pharmacotherapy. 59 (7): 408–414. doi:10.1016/j.biopha.2005.02.003. PMID 16084060.
- Danka Pericic; Maja Jazvinscak Jembrek; Dubravka Svob Strac; Josipa Lazic & Ivana Rajcan Spoljaric (January 2005). "Enhancement of benzodiazepine binding sites following chronic treatment with flumazenil". European Journal of Pharmacology. 507 (1–3): 7–13. doi:10.1016/j.ejphar.2004.10.057. PMID 15659288.
- Danka Pericic; Josipa Lazic; Maja Jazvinscak Jembrek; Dubravka Svob Strac & Ivana Rajcan (December 2004). "Chronic exposure of cells expressing recombinant GABAA receptors to benzodiazepine antagonist flumazenil enhances the maximum number of benzodiazepine binding sites". Life sciences. 76 (3): 303–317. doi:10.1016/j.lfs.2004.07.013. PMID 15531382.
- Maja Jazvinscak Jembrek; Dubravka Svob Strac; Josipa Vlainic & Danka Pericic (July 2008). "The role of transcriptional and translational mechanisms in flumazenil-induced up-regulation of recombinant GABA(A) receptors". Neuroscience Research. 61 (3): 234–241. doi:10.1016/j.neures.2008.03.005. PMID 18453026. S2CID 9033302.
- L. Saxon; S. Borg & A. J. Hiltunen (August 2010). "Reduction of aggression during benzodiazepine withdrawal: effects of flumazenil". Pharmacology Biochemistry and Behavior. 96 (2): 148–151. doi:10.1016/j.pbb.2010.04.023. PMID 20451546. S2CID 41351863.
- Faccini, Marco; Leone, Roberto; Opri, Sibilla; Casari, Rebecca; Resentera, Chiara; Morbioli, Laura; Conforti, Anita; Lugoboni, Fabio (October 2016). "Slow subcutaneous infusion of flumazenil for the treatment of long-term, high-dose benzodiazepine users: a review of 214 cases". Journal of Psychopharmacology (Oxford, England). 30 (10): 1047–1053. doi:10.1177/0269881116647505. ISSN 1461-7285. PMID 27166362. S2CID 27167585.
- Tamburin, Stefano; Faccini, Marco; Casari, Rebecca; Federico, Angela; Morbioli, Laura; Franchini, Enrica; Bongiovanni, Luigi Giuseppe; Lugoboni, Fabio (October 2017). "Low risk of seizures with slow flumazenil infusion and routine anticonvulsant prophylaxis for high-dose benzodiazepine dependence". Journal of Psychopharmacology (Oxford, England). 31 (10): 1369–1373. doi:10.1177/0269881117714050. ISSN 1461-7285. PMID 28613124. S2CID 42432213.
- Hood, Sean David; Norman, Amanda; Hince, Dana Adelle; Melichar, Jan Krzysztof; Hulse, Gary Kenneth (February 2014). "Benzodiazepine dependence and its treatment with low dose flumazenil". British Journal of Clinical Pharmacology. 77 (2): 285–294. doi:10.1111/bcp.12023. ISSN 1365-2125. PMC 4014019. PMID 23126253.
- Hadingham, K. L.; Garrett, E. M.; Wafford, K. A.; Bain, C.; Heavens, R. P.; Sirinathsinghji, D. J.; Whiting, P. J. (February 1996). "Cloning of cDNAs encoding the human gamma-aminobutyric acid type A receptor alpha 6 subunit and characterization of the pharmacology of alpha 6-containing receptors". Molecular Pharmacology. 49 (2): 253–259. ISSN 0026-895X. PMID 8632757.
- Gunja, Naren (June 2013). "The clinical and forensic toxicology of Z-drugs". Journal of Medical Toxicology. 9 (2): 155–162. doi:10.1007/s13181-013-0292-0. ISSN 1937-6995. PMC 3657020. PMID 23404347.
- Thornton, Stephen L.; Negus, Elezer; Carstairs, Shaun D. (November 2013). "Pediatric zolpidem ingestion demonstrating zero-order kinetics treated with flumazenil". Pediatric Emergency Care. 29 (11): 1204–1206. doi:10.1097/PEC.0b013e3182aa139c. ISSN 1535-1815. PMID 24196090. S2CID 34655918.
- Lheureux, P.; Debailleul, G.; De Witte, O.; Askenasi, R. (March 1990). "Zolpidem intoxication mimicking narcotic overdose: response to flumazenil". Human & Experimental Toxicology. 9 (2): 105–107. doi:10.1177/096032719000900209. ISSN 0960-3271. PMID 2111156. S2CID 34525063.
Other
- Romazicon product information, Roche USA
External links
 Media related to Flumazenil at Wikimedia Commons
Media related to Flumazenil at Wikimedia Commons- Flumazenil drug label/data at Daily Med from U.S. National Library of Medicine, National Institutes of Health.
