Shigellosis
Shigellosis is an infection of the intestines caused by Shigella bacteria.[1][3] Symptoms generally start one to two days after exposure and include diarrhea, fever, abdominal pain, and feeling the need to pass stools even when the bowels are empty.[1] The diarrhea may be bloody.[1] Symptoms typically last five to seven days and it may take several months before bowel habits return entirely to normal.[1] Complications can include reactive arthritis, sepsis, seizures, and hemolytic uremic syndrome.[1]
| Shigellosis | |
|---|---|
| Other names | Bacillary dysentery, Marlow syndrome |
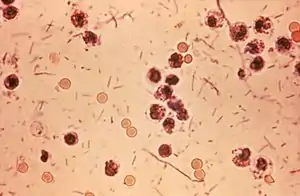 | |
| Shigella seen in a stool sample | |
| Specialty | Infectious disease |
| Symptoms | Diarrhea, fever, abdominal pain[1] |
| Complications | Reactive arthritis, sepsis, seizures, hemolytic uremic syndrome[1] |
| Usual onset | 1–2 days post exposure[1] |
| Duration | Usually 5–7 days[1] |
| Causes | Shigella[1] |
| Diagnostic method | Stool culture[1] |
| Prevention | Handwashing[1] |
| Treatment | Drinking fluids and rest[1] |
| Medication | Antibiotics (severe cases)[1] |
| Frequency | >80 million[2] |
| Deaths | 700,000[2] |
Shigellosis is caused by four specific types of Shigella.[2] These are typically spread by exposure to infected feces.[1] This can occur via contaminated food, water, or hands or sexual contact.[1][4] Contamination may be spread by flies or when changing diapers (nappies).[1] Diagnosis is by stool culture.[1]
The risk of infection can be reduced by properly washing the hands.[1] There is no vaccine.[1] Shigellosis usually resolves without specific treatment.[1] Sufficient fluids by mouth and rest is recommended.[1] Bismuth subsalicylate may help with the symptoms; however, medications that slow the bowels such as loperamide are not recommended.[1] In severe cases antibiotics may be used but resistance is common.[1][5] Commonly used antibiotics include ciprofloxacin and azithromycin.[1]
Globally shigellosis occurs in at least 80 million people and results in about 700,000 deaths a year.[2] Most cases occur in the developing world.[2] Young children are most commonly affected.[1] Outbreaks of disease may occur in childcare settings and schools.[1] It is also relatively common among travelers.[1] In the United States about half a million cases occur a year.[1]
Signs and symptoms
Signs and symptoms may range from mild abdominal discomfort to full-blown dysentery characterized by cramps, diarrhea, with slimy-consistent stools, fever, blood, pus, or mucus in stools or tenesmus.[6][7] Onset time is 12 to 96 hours, and recovery takes 5 to 7 days.[8] Infections are associated with mucosal ulceration, rectal bleeding, and drastic dehydration. Reactive arthritis and hemolytic uremic syndrome are possible sequelae that have been reported in the aftermath of shigellosis.
Cause
Bacteria
Shigellosis is caused by a bacterial infection with Shigella,[1] a bacterium that is genetically similar to and was once classified as E. coli.[10] There are three serogroups and one serotype of Shigella:
- Shigella flexneri
- Shigella boydii
- Shigella dysenteriae and
- Shigella sonnei (serotype)[1]
The probability of being infected by any given strain of Shigella varies around the world. For instance, S. sonnei is the most common in the United States, while S. dysenteriae and S. boydii are rare in the U.S.[1]
Mechanism
Upon ingestion, the bacteria pass through the gastrointestinal tract until they reach the small intestine. There they begin to multiply until they reach the large intestine.[13] In the large intestine, the bacteria cause cell injury and the beginning stages of Shigellosis via two main mechanisms: direct invasion of epithelial cells in the large intestine and production of enterotoxin 1 and enterotoxin 2.[13]
Unlike other bacteria, Shigella is not destroyed by the gastric acid in the stomach. As a result, it takes only 10 to 200 cells to cause an infection.[13] This infectious dose is several order of magnitudes smaller than that of other species of bacteria (e.g. cholera, caused by the bacterium Vibrio cholerae, has an infectious dose between 108 and 1011 cells).[14]
Diagnosis
The diagnosis of shigellosis is made by isolating the organism from diarrheal fecal sample cultures. Shigella species are negative for motility and are generally not lactose fermenters, but S. sonnei can ferment lactose.[15] They typically do not produce gas from carbohydrates (with the exception of certain strains of S. flexneri) and tend to be overall biochemically inert. Shigella should also be urea hydrolysis negative. When inoculated to a triple sugar iron slant, they react as follows: K/A, gas -, and H2S -. Indole reactions are mixed, positive and negative, with the exception of S. sonnei, which is always indole negative. Growth on Hektoen enteric agar produces bluish-green colonies for Shigella and bluish-green colonies with black centers for Salmonella.
Prevention
Simple precautions can be taken to prevent getting shigellosis: wash hands before handling food and thoroughly cook all food before eating. The primary prevention methods are improved sanitation and personal and food hygiene, but a low-cost and efficacious vaccine would complement these methods.[16]
Since shigellosis is spread very quickly among children, keeping infected children out of daycare for 24 hours after their symptoms have disappeared, will decrease the occurrence of shigellosis in daycares.[17]
Vaccine
Currently, no licensed vaccine targeting Shigella exists. Several vaccine candidates for Shigella are in various stages of development including live attenuated, conjugate, ribosomal, and proteosome vaccines.[16][18][19] Shigella has been a longstanding World Health Organization target for vaccine development, and sharp declines in age-specific diarrhea/dysentery attack rates for this pathogen indicate that natural immunity does develop following exposure; thus, vaccination to prevent the disease should be feasible. Shigellosis is resistant to many antibiotics used to treat the disease,[20] so vaccination is an important part of the strategy to reduce morbidity and mortality.[16]
Treatment
Treatment consists mainly of replacing fluids and salts lost because of diarrhea. Replacement by mouth is satisfactory for most people, but some may need to receive fluids intravenously. Antidiarrheal drugs (such as diphenoxylate or loperamide) may prolong the infection and should not be used.[21]
Antibiotics
Antibiotics should only be used in severe cases or for certain populations with mild symptoms (elderly, immunocompromised, food service industry workers, child care workers). For Shigella-associated diarrhea, antibiotics shorten the length of infection,[22] but they are usually avoided in mild cases because many Shigella strains are becoming resistant to common antibiotics.[23] Furthermore, effective medications are often in short supply in developing countries, which carry the majority of the disease burden from Shigella. Antidiarrheal agents may worsen the sickness, and should be avoided.[24]
In most cases, the disease resolves within four to eight days without antibiotics. Severe infections may last three to six weeks. Antibiotics, such as trimethoprim-sulfamethoxazole, ciprofloxacin may be given when the person is very young or very old, when the disease is severe, or when the risk of the infection spreading to other people is high. Additionally, ampicillin (but not amoxicillin) was effective in treating this disease previously, but now the first choice of drug is pivmecillinam.[25]
Epidemiology
Insufficient data exist,[26] but it is estimated to have caused the death of 34,000 children under the age of five in 2013, and 40,000 deaths in people over five years of age.[16] Shigella also causes about 580,000 cases annually among travelers and military personnel from industrialized countries.[27]
An estimated 500,000 cases of shigellosis occur annually in the United States.[20] Infants, the elderly, and the critically ill are susceptible to the most severe symptoms of disease, but all humans are susceptible to some degree. Individuals with acquired immune deficiency syndrome (AIDS) are more frequently infected with Shigella.[28] Shigellosis is a more common and serious condition in the developing world; fatality rates of shigellosis epidemics in developing countries can be 5–15%.[29]
Orthodox Jewish communities (OJCs) are a known risk group for shigellosis; Shigella sonnei is cyclically epidemic in these communities in Israel, with sporadic outbreaks occurring elsewhere in among these communities. "Through phylogenetic and genomic analysis, we showed that strains from outbreaks in OJCs outside of Israel are distinct from strains in the general population and relate to a single multidrug-resistant sublineage of S. sonnei that prevails in Israel. Further Bayesian phylogenetic analysis showed that this strain emerged approximately 30 years ago, demonstrating the speed at which antimicrobial drug–resistant pathogens can spread widely through geographically dispersed, but internationally connected, communities."[30]
References
- "General Information| Shigella – Shigellosis | CDC". www.cdc.gov. 3 August 2016. Archived from the original on 16 April 2017. Retrieved 20 April 2017.
- Guidelines for the control of shigellosis, including epidemics due to Shigella dysenteriae type 1 (PDF). WHO. 2005. p. 2. ISBN 978-9241593304. Archived (PDF) from the original on 21 August 2017. Retrieved 20 April 2017.
- "Factsheet about shigellosis". European Centre for Disease Prevention and Control.
- Antibiotic Resistance Threats in the United States, 2019 (PDF). CDC. 2019. p. 9.
- "Update – CDC Recommendations for Managing and Reporting Shigella Infections with Possible Reduced Susceptibility to Ciprofloxacin". emergency.cdc.gov. 7 June 2018. Retrieved 16 June 2018.
- "Shigellosis". The Merck Manual Home Health Handbook. Archived from the original on 4 January 2012. Retrieved 10 February 2012.
- Niyogi, SK (April 2005). "Shigellosis". Journal of Microbiology (Seoul, Korea). 43 (2): 133–43. PMID 15880088.
- "Symptoms of Shigella Infection". About Shigella. Marler Clark. Archived from the original on 8 January 2012. Retrieved 10 February 2012.
- "Diarrhoeal Diseases: Shigellosis". Initiative for Vaccine Research. World Health Organization. Archived from the original on 15 December 2008. Retrieved 11 May 2012.
- Devanga Ragupathi, NK; Muthuirulandi Sethuvel, DP; Inbanathan, FY; Veeraraghavan, B (21 January 2018). "Accurate differentiation of Escherichia coli and Shigella serogroups: challenges and strategies". New Microbes New Infect. 21: 58–62. doi:10.1016/j.nmni.2017.09.003. PMC 5711669. PMID 29204286.
- "Shigellosis (Bacillary Dysentery)". Merck Manual Professional Version. Retrieved 16 March 2018.
- Bowen, Anna (31 May 2017). "Travelers' Health, Chapter 3, Shigellosis (CDC)". Retrieved 17 March 2018.
- Aslam, A; Gossman, WG (14 February 2018). Shigella (Shigellosis). Treasure Island, FL: StatPearls. PMID 29493962.
- Nelson, EJ; Harris, JB; Glenn Morris, Jr., J; Calderwood, SB; Camilli, A (October 2009). "Cholera transmission: the host, pathogen and bacteriophage dynamic". Nat Rev Microbiol. 7 (10): 693–702. doi:10.1038/nrmicro2204. PMC 3842031. PMID 19756008.
- Ito, Hideo; Kido, Nobuo; Arakawa, Yoshichika; Ohta, Michio; Sugiyama, Tsuyoshi; Kato, Nobuo (1991). "Possible mechanisms underlying the slow lactose fermentation phenotype in Shigella spp". Applied and Environmental Microbiology. 57 (10): 2912–7. doi:10.1128/AEM.57.10.2912-2917.1991. PMC 183896. PMID 1746953.
- Mani, Sachin; Wierzba, Thomas; Walker, Richard I. (2016). "Status of vaccine research and development for Shigella". Vaccine. 34 (26): 2887–2894. doi:10.1016/j.vaccine.2016.02.075. PMID 26979135.
- mayo clinic "Shigella infection - Symptoms and causes". Archived from the original on 6 September 2015. Retrieved 14 September 2015.
- "WHO vaccine pipeline tracker". World Health Organization. Archived from the original on 25 July 2016. Retrieved 29 July 2016.
- "Vaccine Research And Development: New strategies for accelerating Shigella vaccine development" (PDF). Weekly Epidemiological Record. 72 (11): 73–80. 14 March 1997. PMID 9115858. Archived (PDF) from the original on 19 May 2009. Retrieved 10 February 2012.
- US Centers for Disease Control and Prevention. "Shigella – Shigellosis". Archived from the original on 24 July 2016. Retrieved 29 July 2016.
- "How can Shigella infections be treated?". Shigellosis: General Information. Centers for Disease Control and Prevention. 17 January 2019. Archived from the original on 8 February 2016.
- Christopher, Prince RH; David, Kirubah V; John, Sushil M; Sankarapandian, Venkatesan; Christopher, Prince RH (2010). "Antibiotic therapy for Shigella dysentery". The Cochrane Database of Systematic Reviews (8): CD006784. doi:10.1002/14651858.CD006784.pub4. PMC 6532574. PMID 20687081.
- Kahsay, AG; Muthupandian, S (30 August 2016). "A review on Sero diversity and antimicrobial resistance patterns of Shigella species in Africa, Asia and South America, 2001-2014". BMC Research Notes. 9 (1): 422. doi:10.1186/s13104-016-2236-7. PMC 5004314. PMID 27576729.
- "How can Shigella infections be treated?". Shigellosis: General Information. Centers for Disease Control and Prevention. Archived from the original on 11 February 2012. Retrieved 11 February 2012.
- Katzung, Bertram G. (2007). Basic and Clinical Pharmacology. New York, NY: McGraw Hill Medical. p. 733. ISBN 978-0-07-145153-6.
- Ram, PK; Crump JA; Gupta SK; Miller MA; Mintz ED (2008). "Analysis of Data Gaps Pertaining to Shigella Infections in Low and Medium Human Development Index Countries, 1984–2005". Epidemiology and Infection. 136 (5): 577–603. doi:10.1017/S0950268807009351. PMC 2870860. PMID 17686195.
- World Health Organization (2006). State of the art of new vaccine research and development (PDF). Archived (PDF) from the original on 4 March 2016.
- Angulo, Frederick J.; Swerdlow, David L. (1995). "Bacterial Enteric Infections in Persons Infected with Human Immunodeficiency Virus". Clinical Infectious Diseases. 21 (Supplement 1): S84–S93. doi:10.1093/clinids/21.supplement_1.s84. PMID 8547518.
- Todar, Kenneth. "Shigella and Shigellosis". Todar's Online Textbook of Bacteriology. Archived from the original on 9 February 2012. Retrieved 10 February 2012.
- Baker, K; et al. (September 2016). "Travel- and Community-Based Transmission of Multidrug-Resistant Shigella sonnei Lineage among International Orthodox Jewish Communities". Emerg Infect Dis. 22 (9): 1545–1553. doi:10.3201/eid2209.151953. PMC 4994374. PMID 27532625.
External links
- CDC's Shigellosis Page
- Vaccine Resource Library: Shigellosis and enterotoxigenic Escherichia coli (ETEC)
| Classification | |
|---|---|
| External resources |