Vitamin B6
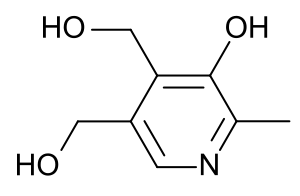
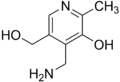
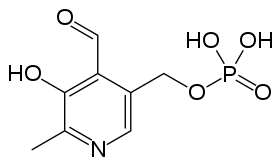
Vitamin B6 is one of the B vitamins, and thus an essential nutrient.[1][2][3][4] The term refers to a group of chemically similar compounds, "vitamers", which can be interconverted in biological systems. Its active form, pyridoxal 5′-phosphate, serves as a coenzyme in some 100 enzyme reactions in amino acid, glucose, and lipid metabolism.[1][2][3]
| Vitamin B6 | |
|---|---|
| Drug class | |
 | |
| Class identifiers | |
| Use | Vitamin B6 deficiency |
| ATC code | A11HA02 |
| Biological target | enzyme cofactor |
| Clinical data | |
| Drugs.com | International Drug Names |
| External links | |
| MeSH | D025101 |
| In Wikidata | |
Forms
Absorbed pyridoxamine is converted to PMP by pyridoxal kinase, which is further converted to PLP by pyridoxamine-phosphate transaminase or pyridoxine 5′-phosphate oxidase which also catalyzes the conversion of PNP to PLP.[3] Pyridoxine 5′-phosphate oxidase is dependent on flavin mononucleotide (FMN) as a cofactor produced from riboflavin (vitamin B2).
- Pyridoxine (PN), the form most commonly given as vitamin B6 supplement
- Pyridoxine 5′-phosphate (P5P)
- Pyridoxal (PL)
- Pyridoxal 5′-phosphate (PLP), the metabolically active form
- Pyridoxamine (PM)
- Pyridoxamine 5′-phosphate (PMP)
- 4-Pyridoxic acid (PA), the catabolite which is excreted in urine
- Pyritinol
All forms except pyridoxic acid and pyritinol can be interconverted.[3] Pyritinol is a semi-synthetic derivative of pyridoxine, where two pyridoxine moieties are bound by a disulfide bridge.
Functions
PLP, the metabolically active form of vitamin B6, is involved in many aspects of macronutrient metabolism, neurotransmitter synthesis, histamine synthesis, hemoglobin synthesis and function, and gene expression. PLP generally serves as a coenzyme (cofactor) for many reactions including decarboxylation, transamination, racemization, elimination, replacement, and beta-group interconversion.[2][3][5]
Amino acid metabolism
- PLP is a cofactor in the biosynthesis of five important neurotransmitters: serotonin, dopamine, epinephrine, norepinephrine, and gamma-aminobutyric acid (GABA). PLP is also involved in the synthesis of histamine.
- Transaminases break down amino acids with PLP as a cofactor. The proper activity of these enzymes is crucial for the process of moving amine groups from one amino acid to another.
- Serine racemase which synthesizes the neuromodulator D-serine from its enantiomer is a PLP-dependent enzyme.
- PLP is a coenzyme needed for the proper function of the enzymes cystathionine synthase and cystathionase. These enzymes catalyze reactions in the catabolism of methionine. Part of this pathway (the reaction catalyzed by cystathionase) also produces cysteine.
- Selenomethionine is the primary dietary form of selenium. PLP is needed as a cofactor for the enzymes that allow selenium to be used from the dietary form. PLP also plays a cofactor role in releasing selenium from selenohomocysteine to produce hydrogen selenide, which can then be used to incorporate selenium into selenoproteins.
- PLP is required for the conversion of tryptophan to niacin, so low vitamin B6 status impairs this conversion.[5]
Glucose metabolism
PLP is a required coenzyme of glycogen phosphorylase, the enzyme necessary for glycogenolysis to occur.[5] PLP can catalyze transamination reactions that are essential for providing amino acids as a substrate for gluconeogenesis.
Lipid metabolism
PLP is an essential component of enzymes that facilitate the biosynthesis of sphingolipids.[5] Particularly, the synthesis of ceramide requires PLP. In this reaction, serine is decarboxylated and combined with palmitoyl-CoA to form sphinganine, which is combined with a fatty acyl-CoA to form dihydroceramide. Dihydroceramide is then further desaturated to form ceramide. In addition, the breakdown of sphingolipids is also dependent on vitamin B6 because sphingosine-1-phosphate lyase, the enzyme responsible for breaking down sphingosine-1-phosphate, is also PLP-dependent.
Hemoglobin synthesis and function
PLP aids in the synthesis of hemoglobin, by serving as a coenzyme for the enzyme ALA synthase.[6] It also binds to two sites on hemoglobin to enhance the oxygen binding of hemoglobin.[5]
Gene expression
PLP has been implicated in increasing or decreasing the expression of certain genes. Increased intracellular levels of the vitamin lead to a decrease in the transcription of glucocorticoids. Also, vitamin B6 deficiency leads to the increased gene expression of albumin mRNA. Also, PLP influences expression of glycoprotein IIb by interacting with various transcription factors. The result is inhibition of platelet aggregation.[5]
Dietary recommendations
The US National Academy of Medicine updated Dietary Reference Intakes for many vitamins in 1998. Recommended Dietary Allowances (RDAs) increase with age from 1.2 to 1.5 mg/day for women and from 1.3 to 1.7 mg/day for men. The RDA for pregnancy is 1.9 mg/day. The RDA for lactation is 2.0 mg/day. For children ages 1–13 years the RDA increases with age from 0.5 to 1.0 mg/day. As for safety, Tolerable upper intake levels (ULs) for vitamins and minerals are identified when evidence is sufficient. In the case of vitamin B6 the adult UL is set at 100 mg/day.[4]
The European Food Safety Authority (EFSA) refers to the collective set of information as Dietary Reference Values, with Population Reference Intake (PRI) instead of RDA. ULs are defined the same as in US. For women and men ages 15 and older the PRI is set at 1.6 and 1.7 mg/day, respectively. For pregnancy 1.8 mg/day. For lactation 1.7 mg/day. For children ages 1–14 years the PRIs increase with age from 0.6 to 1.4 mg/day.[7] The EFSA also reviewed the safety question and set its UL at 25 mg/day.[8][9]
Safety
Adverse effects have been documented from vitamin B6 dietary supplements, but never from food sources. Even though it is a water-soluble vitamin and is excreted in the urine, doses of pyridoxine in excess of the dietary upper limit (UL) over long periods cause painful and ultimately irreversible neurological problems.[4] The primary symptoms are pain and numbness of the extremities. In severe cases, motor neuropathy may occur with "slowing of motor conduction velocities, prolonged F wave latencies, and prolonged sensory latencies in both lower extremities", causing difficulty in walking. Sensory neuropathy typically develops at doses of pyridoxine in excess of 1,000 mg per day, but adverse effects can occur with much less, so doses over 200 mg are not considered safe. Symptoms among women taking lower doses have been reported.[4]
Labeling
For US food and dietary supplement labeling purposes the amount in a serving is expressed as a percent of Daily Value. For vitamin B6 labeling purposes 100% of the Daily Value was 2.0 mg, but as of May 27, 2016 it was revised to 1.7 mg to bring it into agreement with the adult RDA.[10][11] Compliance with the updated labeling regulations was required by 1 January 2020 for manufacturers with US$10 million or more in annual food sales, and by 1 January 2021 for manufacturers with lower volume food sales.[12][13] A table of the old and new adult daily values is provided at Reference Daily Intake.
Sources
Vitamin B6 is found in a wide variety of foods. The richest sources of vitamin B6 include fish, beef liver and other organ meats, potatoes and other starchy vegetables, and fruit other than citrus. About 75% of vitamin B6 from a mixed diet is bioavailable.[4] Cooking, storage, and processing losses vary, and in some foods may be more than 50% depending on the form of vitamin present in the food.[3] Plant foods lose the least during processing, as they contain mostly pyridoxine, which is far more stable than the pyridoxal or pyridoxamine found in animal foods. For example, milk can lose 30–70% of its vitamin B6 content when dried.[5] Vitamin B6 is found in the germ and aleurone layer of grains, and milling results in the reduction of this vitamin in white flour.
| Source[1] | Amount (mg serving) |
|---|---|
| Beef liver, pan fried, 3 ounces | 0.9 |
| Tuna, yellowfin, fresh, cooked, 3 ounces | 0.9 |
| Pork 4 ounces | 0.85 |
| Salmon, sockeye, cooked, 3 ounces | 0.6 |
| Chicken breast, roasted, 3 ounces | 0.5 |
| Chickpeas, canned, 1/2 cup | 0.55 |
| Banana, 1 medium | 0.4 |
| Hazelnuts, chopped, 1/2 cup | 0.32 |
| Sweet potato, medium | 0.32 |
| Source[1] | Amount (mg / serving) |
|---|---|
| Ground beef, patty, 85% lean, broiled, 3 ounces | 0.3 |
| Cottage cheese, 1% low-fat, 1 cup | 0.2 |
| Potatoes, boiled, 1/2 cup | 0.2 |
| Squash, winter, baked, 1/2 cup | 0.2 |
| Rice, white, long-grain, enriched, cooked, 1 cup | 0.1 |
| Nuts, mixed, dry-roasted, 1 ounce | 0.1 |
| Raisins, seedless, 1/2 cup | 0.1 |
| Onions, chopped, 1/2 cup | 0.1 |
| Tofu, firm, 1/2 cup | 0.1 |
| Source[1] | Amount (mg / serving) |
|---|---|
| Corn grits, 1.0 cup | 0.12 |
| Milk, one cup | 0.12 |
| Corn, canned, 1/2 cup | 0.1 |
| Almonds, 1 ounce | 0.1 |
| Cheese, one cup, diced | 0.1 |
| Soy beans, one cup | 0.1 |
| Yogurt, 6 ounces | 0.08 |
| Chicken egg one | 0.07 |
| Bread, one slice | 0.02 |
Absorption and excretion
Vitamin B6 is absorbed in the jejunum and ileum by passive diffusion. With the capacity for absorption being so great, animals are able to absorb quantities much greater than necessary for physiological demands. The absorption of pyridoxal phosphate and pyridoxamine phosphate involves their dephosphorylation catalyzed by a membrane-bound alkaline phosphatase. Those products and nonphosphorylated forms in the digestive tract are absorbed by diffusion, which is driven by trapping of the vitamin as 5′-phosphates through the action of phosphorylation (by a pyridoxal kinase) in the jejunal mucosa. The trapped pyridoxine and pyridoxamine are oxidized to pyridoxal phosphate in the tissue.[5]
The products of vitamin B6 metabolism are excreted in the urine, the major product of which is 4-pyridoxic acid. An estimated 40–60% of ingested vitamin B6 is oxidized to 4-pyridoxic acid. Several studies have shown that 4-pyridoxic acid is undetectable in the urine of vitamin B6-deficient subjects, making it a useful clinical marker to assess the vitamin B6 status of an individual.[5] Other products of vitamin B6 metabolism excreted in the urine when high doses of the vitamin have been given include pyridoxal, pyridoxamine, and pyridoxine and their phosphates. A small amount of vitamin B6 is also excreted in the feces.
Deficiency
Signs and symptoms
The classic clinical syndrome for vitamin B6 deficiency is a seborrhoeic dermatitis-like eruption, atrophic glossitis with ulceration, angular cheilitis, conjunctivitis, intertrigo, and neurologic symptoms of somnolence, confusion, and neuropathy (due to impaired sphingosine synthesis) and microcytic anemia (due to impaired heme synthesis).[1]
Less severe cases present with metabolic disease associated with insufficient activity of the coenzyme PLP. The most prominent of the lesions is due to impaired tryptophan–niacin conversion. This can be detected based on urinary excretion of xanthurenic acid after an oral tryptophan load. Vitamin B6 deficiency can also result in impaired transsulfuration of methionine to cysteine. The PLP-dependent transaminases and glycogen phosphorylase provide the vitamin with its role in gluconeogenesis, so deprivation of vitamin B6 results in impaired glucose tolerance.[5]
Diagnosis
The assessment of vitamin B6 status is essential, as the clinical signs and symptoms in less severe cases are not specific.[14] The three biochemical tests most widely used are the activation coefficient for the erythrocyte enzyme aspartate aminotransferase, plasma PLP concentrations, and the urinary excretion of vitamin B6 degradation products, specifically urinary PA. Of these, plasma PLP is probably the best single measure, because it reflects tissue stores. Plasma PLP less than 10 nmol/l is indicative of vitamin B6 deficiency.[15] A PLP concentration greater than 20 nmol/l has been chosen as a level of adequacy for establishing Estimated Average Requirements and Recommended Daily Allowances in the USA.[4] Urinary PA is also an indicator of vitamin B6 deficiency; levels of less than 3.0 mmol/day is suggestive of vitamin B6 deficiency.[15]
The classic syndrome for vitamin B6 deficiency is rare, even in developing countries. A handful of cases were seen between 1952 and 1953, particularly in the United States, and occurred in a small percentage of infants who were fed a formula lacking in pyridoxine.[16]
Causes
A deficiency of vitamin B6 alone is relatively uncommon and often occurs in association with other vitamins of the B complex. The elderly and alcoholics have an increased risk of vitamin B6 deficiency, as well as other micronutrient deficiencies.[3] Evidence exists for decreased levels of vitamin B6 in women with type 1 diabetes and in patients with systemic inflammation, liver disease, rheumatoid arthritis, and those infected with HIV.[17][18] Use of oral contraceptives and treatment with certain anticonvulsants, isoniazid, cycloserine, penicillamine, and hydrocortisone negatively impact vitamin B6 status.[1][19][20] Hemodialysis reduces vitamin B6 plasma levels.[21]
Overconsumption of seeds from Ginkgo biloba can deplete vitamin B6, because the ginkgotoxin is an anti-vitamin. Symptoms include vomiting and generalized convulsions. Ginkgo seed poisoning can be treated with vitamin B6.[22]
History
In 1934, the Hungarian physician Paul György discovered a substance that was able to cure a skin disease in rats (dermatitis acrodynia). He named this substance vitamin B6.[23][24] In 1938, Richard Kuhn was awarded the Nobel Prize in Chemistry for his work on carotenoids and vitamins, specifically B2 and B6.[25] Also in 1938, Samuel Lepkovsky isolated vitamin B6 from rice bran.[26] A year later, Stanton A. Harris and Karl August Folkers determined the structure of pyridoxine, and then in 1942 Esmond Emerson Snell developed a microbiological growth assay that led to the characterization of pyridoxamine, the animated product of pyridoxine, and pyridoxal, the formyl derivative of pyridoxine. Further studies showed that pyridoxal, pyridoxamine, and pyridoxine have largely equal activity in animals and owe their vitamin activity to the ability of the organism to convert them into the enzymatically active form pyridoxal-5-phosphate.[26]
See also
References
- "Facts about Vitamin B6 Fact Sheet for Health Professionals". Office of Dietary Supplements at National Institutes of Health. 24 February 2020. Retrieved 5 February 2021.
- "Vitamin B6". Micronutrient Information Center, Linus Pauling Institute, Oregon State University, Corvallis, OR. May 2014. Archived from the original on 2018-03-14. Retrieved 7 March 2017.
- Da Silva VR, Gregory III JF (2020). "Vitamin B6". In BP Marriott, DF Birt, VA Stallings, AA Yates (eds.). Present Knowledge in Nutrition, Eleventh Edition. London, United Kingdom: Academic Press (Elsevier). pp. 225–38. ISBN 978-0-323-66162-1.
- Institute of Medicine (1998). "Vitamin B6". Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: The National Academies Press. pp. 150–195. doi:10.17226/6015. ISBN 978-0-309-06554-2. LCCN 00028380. OCLC 475527045. PMID 23193625.
- Combs GF (2007). The Vitamins: Fundamental Aspects in Nutrition and Health (3rd ed.). San Diego: Elsevier Academic Press. pp. 320–324. ISBN 978-0-8121-0661-9. LCCN 2007026776. OCLC 150255807.
- Erskine PT, Coates L, Butler D, Youell JH, Brindley AA, Wood SP, et al. (August 2003). "X-ray structure of a putative reaction intermediate of 5-aminolaevulinic acid dehydratase". The Biochemical Journal. 373 (Pt 3): 733–8. doi:10.1042/bj20030513. PMC 1223560. PMID 12777167.
- "Overview on Dietary Reference Values for the EU population as derived by the EFSA Panel on Dietetic Products, Nutrition and Allergies" (PDF). 2017. Archived (PDF) from the original on 2017-08-28.
- "Tolerable Upper Intake Levels For Vitamins And Minerals" (PDF). European Food Safety Authority. 2006. Archived (PDF) from the original on 2017-09-19.
- Scientific Panel on Food Additives, Flavourings, Processing Aids and Materials in Contact with Food (2008). "Opinion on Pyridoxal 5′-phosphate as a source for vitamin B6 added for nutritional purposes in food supplements". The EFSA Journal. 760: 1–13. doi:10.2903/j.efsa.2008.760.CS1 maint: multiple names: authors list (link)
- "Federal Register May 27, 2016 Food Labeling: Revision of the Nutrition and Supplement Facts Labels" (PDF). Archived (PDF) from the original on 2017-09-22.
- "Daily Value Reference of the Dietary Supplement Label Database (DSLD)". Dietary Supplement Label Database (DSLD). Retrieved 16 May 2020.
- "Changes to the Nutrition Facts Label". U.S. Food and Drug Administration (FDA). 27 May 2016. Retrieved 16 May 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "Industry Resources on the Changes to the Nutrition Facts Label". U.S. Food and Drug Administration (FDA). 21 December 2018. Retrieved 16 May 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Gibson RS (2005). "Assessment of vitamin B6 status". Principles of Nutritional Assessment (2nd ed.). New York: Oxford University Press. pp. 575–594. ISBN 978-0-19-517169-3. LCCN 2004054778. OCLC 884490740.
- Ueland PM, Ulvik A, Rios-Avila L, Midttun Ø, Gregory JF (2015). "Direct and Functional Biomarkers of Vitamin B6 Status". Annu Rev Nutr. 35: 33–70. doi:10.1146/annurev-nutr-071714-034330. PMC 5988249. PMID 25974692.
- Menkes JH (1980). Textbook of Child Neurology (2nd ed.). Philadelphia: Henry Kimpton Publishers. p. 486. ISBN 978-0-8121-0661-9. LCCN 79010975. OCLC 925196268.
- Massé PG, Boudreau J, Tranchant CC, Ouellette R, Ericson KL (February 2012). "Type 1 diabetes impairs vitamin B(6) metabolism at an early stage of women's adulthood". Applied Physiology, Nutrition, and Metabolism. 37 (1): 167–75. doi:10.1139/h11-146. PMID 22288928.
- Ulvik A, Midttun Ø, Pedersen ER, Eussen SJ, Nygård O, Ueland PM (July 2014). "Evidence for increased catabolism of vitamin B-6 during systemic inflammation". The American Journal of Clinical Nutrition. 100 (1): 250–5. doi:10.3945/ajcn.114.083196. PMID 24808485.
- Wilson SM, Bivins BN, Russell KA, Bailey LB (October 2011). "Oral contraceptive use: impact on folate, vitamin B₆, and vitamin B₁₂ status". Nutrition Reviews. 69 (10): 572–83. doi:10.1111/j.1753-4887.2011.00419.x. PMID 21967158.
- Schwaninger M, Ringleb P, Winter R, Kohl B, Fiehn W, Rieser PA, Walter-Sack I (March 1999). "Elevated plasma concentrations of homocysteine in antiepileptic drug treatment". Epilepsia. 40 (3): 345–50. doi:10.1111/j.1528-1157.1999.tb00716.x. PMID 10080517.
- Corken M, Porter J (September 2011). "Is vitamin B(6) deficiency an under-recognized risk in patients receiving haemodialysis? A systematic review: 2000-2010". Nephrology. 16 (7): 619–25. doi:10.1111/j.1440-1797.2011.01479.x. PMID 21609363.
- Mei N, Guo X, Ren Z, Kobayashi D, Wada K, Guo L (January 2017). "Review of Ginkgo biloba-induced toxicity, from experimental studies to human case reports". J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 35 (1): 1–28. doi:10.1080/10590501.2016.1278298. PMC 6373469. PMID 28055331.
- György P (1934). "Vitamin B2 and the Pellagra-like Dermatitis in Rats". Nature. 133 (3361): 498–9. doi:10.1038/133498a0.
- György P, Eckardt RE (September 1940). "Further investigations on vitamin B(6) and related factors of the vitamin B(2) complex in rats. Parts I and II". The Biochemical Journal. 34 (8–9): 1143–54. doi:10.1042/bj0341143. PMC 1265394. PMID 16747297.
- "The Nobel Prize in Chemistry 1938". Nobelprize.org. Retrieved 5 July 2018.
- Rosenberg IH (2012). "A history of the isolation and identification of vitamin B(6)". Ann Nutr Metab. 61 (3): 236–8. doi:10.1159/000343113. PMID 23183295.
External links
- The B6 database A database of B6-dependent enzymes at University of Parma
- Vitamin+B6 at the US National Library of Medicine Medical Subject Headings (MeSH)