Coronary artery bypass surgery
Coronary artery bypass surgery, also known as coronary artery bypass graft (CABG, pronounced "cabbage") surgery, and colloquially heart bypass or bypass surgery, is a surgical procedure to restore normal blood flow to an obstructed coronary artery. A normal coronary artery transports blood to the heart muscle itself, not through the main circulatory system.
| Coronary artery bypass surgery | |
|---|---|
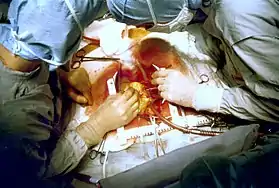
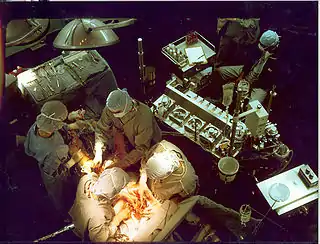 Early in a coronary artery bypass operation, during vein harvesting from the legs (left of image) and the establishment of cardiopulmonary bypass by placement of an aortic cannula (bottom of image). The perfusionist and heart-lung machine are on the upper right. The patient's head (not seen) is at the bottom. | |
| Other names | Coronary artery bypass graft |
| ICD-10-PCS | 021209W |
| ICD-9-CM | 36.1 |
| MeSH | D001026 |
| MedlinePlus | 002946 |
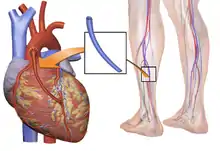
There are two main approaches. In one, the left internal thoracic artery, LITA (also called left internal mammary artery, LIMA) is diverted to the left anterior descending branch of the left coronary artery. In this method, the artery is "pedicled" which means it is not detached from the origin. In the other, a great saphenous vein is removed from a leg; one end is attached to the aorta or one of its major branches, and the other end is attached to the obstructed artery immediately after the obstruction to restore blood flow.
CABG is performed to relieve angina unsatisfactorily controlled by maximum tolerated anti-ischemic medication, prevent or relieve left ventricular dysfunction, and/or reduce the risk of death. CABG does not prevent myocardial infarction (heart attack). This surgery is usually performed with the heart stopped, necessitating the usage of cardiopulmonary bypass. However, two alternative techniques are also available, allowing CABG to be performed on a beating heart either without using the cardiopulmonary bypass, a procedure referred to as "off-pump" surgery, or performing beating surgery using partial assistance of the cardiopulmonary bypass, a procedure referred to as "on-pump beating" surgery. The latter procedure offers the advantages of the on-pump stopped and off-pump while minimizing their respective side-effects.
CABG is often indicated when coronary arteries have a 50 to 99 percent obstruction. The obstruction being bypassed is typically due to arteriosclerosis, atherosclerosis, or both. Arteriosclerosis is characterized by thickening, loss of elasticity, and calcification of the arterial wall, most often resulting in a generalized narrowing in the affected coronary artery. Atherosclerosis is characterized by yellowish plaques of cholesterol, lipids, and cellular debris deposited into the inner layer of the wall of a large or medium-sized coronary artery, most often resulting in a partial obstruction in the affected artery. Either condition can limit blood flow if it causes a cross-sectional narrowing of at least 50%.
Terminology

There are many variations in terminology, in which one or more of "artery", "bypass" or "graft" is left out. The most frequently used acronym for this type of surgery is CABG (pronounced 'cabbage'),[1] pluralized as CABGs (pronounced 'cabbages'). Initially the term aortocoronary bypass (ACB) was more popularly used to describe this procedure.[2] CAGS (coronary artery graft surgery, pronounced phonetically) should not be confused with coronary angiography (CAG).
Number of arteries bypassed
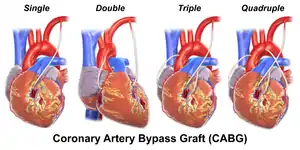
The terms single bypass, double bypass, triple bypass, quadruple bypass and quintuple bypass refer to the number of coronary arteries bypassed in the procedure. In other words, a double bypass means two coronary arteries are bypassed (e.g., the left anterior descending (LAD) coronary artery and right coronary artery (RCA)); a triple bypass means three vessels are bypassed (e.g., LAD, RCA and left circumflex artery (LCX)); a quadruple bypass means four vessels are bypassed (e.g., LAD, RCA, LCX and first diagonal artery of the LAD) while quintuple means five. Left main coronary artery obstruction requires two bypasses, one to the LAD and one to the LCX.
A coronary artery may be unsuitable for bypass grafting if it is small (< 1 mm or < 1.5 mm), heavily calcified, or located within the heart muscle rather than on the surface. A single obstruction of the left main coronary artery is associated with a higher risk for a cardiac death and usually receives a double bypass.
The surgeon reviews the coronary angiogram prior to surgery and identifies the number of obstructions, the percent obstruction of each, and the suitability of the arteries beyond the obstruction(s) as targets. The presumed number of bypass grafts needed as well as the location for graft attachment is determined in a preliminary fashion prior to surgery, but the final decision as to number and location is made during surgery by direct examination of the heart.
Efficacy
- The 2004 ACC/AHA CABG guidelines state CABG is the preferred treatment for:[3]
- Disease of the left main coronary artery (LMCA).
- Disease of all three coronary arteries (LAD, LCX and RCA).
- Diffuse disease not amenable to treatment with a PCI.
- The 2005 ACC/AHA guidelines further state that CABG is the preferred treatment with other high-risk patients such as those with severe ventricular dysfunction (i.e. low ejection fraction), or diabetes mellitus.[3]
- Bypass surgery can provide relief of angina when the location of partial obstructions precludes improving blood flow with stents.
- There is no survival benefit with bypass surgery vs. medical therapy in stable angina patients.
- Bypass surgery does not prevent future myocardial infarctions.[4]
Age per se is not a factor in determining risk vs benefit of CABG.[5]
Prognosis following CABG depends on a variety of factors, and successful grafts typically last 8–15 years. In general, CABG improves the chances of survival of patients who are at high risk (generally triple or higher bypass), though statistically after about five years the difference in survival rate between those who have had surgery and those treated by drug therapy diminishes. Age at the time of CABG is critical to the prognosis, younger patients with no complicating diseases doing better, while older patients can usually be expected to suffer further blockage of the coronary arteries.[6]
Veins that are used either have their valves removed or are turned around so that the valves in them do not occlude blood flow in the graft. External support may be placed on the vein prior to grafting into the coronary circulation of the patient. LITA grafts are longer-lasting than vein grafts, both because the artery is more robust than a vein and because, being already connected to the arterial tree, the LITA need only be grafted at one end. The LITA is usually grafted to the left anterior descending coronary artery (LAD) because of its superior long-term patency when compared to saphenous vein grafts.[7][8]
Results compared to stent placement
CABG or stent placement is indicated when medical management - anti-angina medications, statins, antihypertensives, smoking cessation, and/or tight blood sugar control in diabetics - do not satisfactorily relieve ischemic symptoms.
- Both PCI and CABG are more effective than medical management at relieving symptoms,[9] (e.g. angina, dyspnea, fatigue).
- CABG is superior to PCI for some patients with multivessel CAD[10][11]
- The Surgery or Stent (SoS) trial was a randomized controlled trial that compared CABG to PCI with bare-metal stents. The SoS trial demonstrated CABG is superior to PCI in multivessel coronary disease.[10]
- The SYNTAX trial was a randomized controlled trial of 1800 patients with multivessel coronary disease, comparing CABG versus PCI using drug-eluting stents (DES). The study found that rates of major adverse cardiac or cerebrovascular events at 12 months were significantly higher in the DES group (17.8% versus 12.4% for CABG; P=0.002).[11] This was primarily driven by higher need for repeat revascularization procedures in the PCI group with no difference in repeat infarctions or survival. Higher rates of strokes were seen in the CABG group.
- The FREEDOM (Future Revascularization Evaluation in Patients With Diabetes Mellitus—Optimal Management of Multivessel Disease) trial will compare CABG and DES in patients with diabetes. The registries of the nonrandomized patients screened for these trials may provide as much robust data regarding revascularization outcomes as the randomized analysis.[12]
- A study comparing the outcomes of all patients in New York state treated with CABG or percutaneous coronary intervention (PCI) demonstrated CABG was superior to PCI with DES in multivessel (more than one diseased artery) coronary artery disease (CAD). Patients treated with CABG had lower rates of death and of death or myocardial infarction than treatment with a coronary stent. Patients undergoing CABG also had lower rates of repeat revascularization.[13] The New York State registry included all patients undergoing revascularization for coronary artery disease, but was not a randomized trial, and so may have reflected other factors besides the method of coronary revascularization.
- A meta-analysis with over 6000 patients showed that coronary artery bypass was associated with lower risk for major adverse cardiac events compared to drug-eluting stenting. However, patients had a higher risk of stroke events.[14]
A 2018 meta-analysis with over 4000 patient cases found hybrid coronary revascularization (LIMA-to-LAD anastomosis combined with percutaneous stents at other atherosclerotic sites) to have significant advantages compared with conventional CABG. Reduced incidence of blood transfusion, reduced hospital stay duration and reduced intubation duration were all reported. In contrast, HCR was found to be significantly more expensive compared to CABG.[15]
Complications
CABG associated
- Postperfusion syndrome (pumphead), a transient neurocognitive impairment associated with cardiopulmonary bypass. Some research shows the incidence is initially decreased by off-pump coronary artery bypass, but with no difference beyond three months after surgery. A neurocognitive decline over time has been demonstrated in people with coronary artery disease regardless of treatment (OPCAB, conventional CABG or medical management). However, a 2009 research study suggests that longer term (over 5 years) cognitive decline is not caused by CABG but is rather a consequence of vascular disease.[16] Loss of mental function is a complication of bypass surgery in elderly people, and might influence procedure cost benefit considerations.[17] Several factors may contribute to immediate cognitive decline. The heart-lung blood circulation system and the surgery itself release a variety of debris, including bits of blood cells, tubing, and plaques. For example, when surgeons clamp and connect the aorta to tubing, resulting emboli block blood flow and cause mini strokes. Other heart surgery factors related to mental damage may be events of hypoxia, high or low body temperature, abnormal blood pressure, irregular heart rhythms, and fever after surgery.[18]
- Nonunion of the sternum; internal thoracic artery harvesting increases the sternum devascularization risk.[19]
- Myocardial infarction due to embolism, hypoperfusion, or graft failure. While remote ischaemic preconditioning (RIPC) reduces the cardiac troponin T (cTnT) release measured at 72 hours after surgery and cardiac troponin I (cTnI) release measured at 48 hours and 72 hours after surgery, it does not reduce reperfusion injury in people undergoing cardiac surgery.[20]
- Late graft stenosis, particularly of saphenous vein grafts due to atherosclerosis causing recurrent angina or myocardial infarction.[21]
- Acute renal failure due to embolism or hypoperfusion.[22][23]
- Stroke, secondary to embolism or hypoperfusion.[24]
- Vasoplegic syndrome, secondary to cardiopulmonary bypass and hypothermia
- Graft failure: grafts last 8–15 years, and then need to be replaced.
- Pneumothorax: An air collection around the lung that compresses the lung[23]
- Hemothorax: Blood in the space around the lungs
- Pericardial tamponade: Blood collection around the heart that compresses the heart and causes poor body and brain perfusion. Chest tubes are placed around the heart and lung to prevent this. If the chest tubes become clogged in the early post operative period when bleeding is ongoing this can lead to pericardial tamponade, pneumothorax or hemothorax.
- Pleural effusion: Fluid in the space around the lungs. This can lead to hypoxia which can slow recovery.
- Pericarditis
- Lower extremity edema, extravasation, inflammation, and eccymoses from vein harvest; entrapment of up to 9 pounds (4.1 kg) of fluid in the extremity is common. This is managed with a thigh length compression stocking, elevation of the limb, and early and frequent slow walking; as well as avoidance of standing in place, sitting, and bending the leg at the knee more than a few degrees.
Open heart surgery associated
- Post-operative atrial fibrillation and atrial flutter.[25]
- Anemia - secondary to blood loss, plus the anemia of inflammation, inflammation being inevitable with opening the chest plus harvesting of leg vein(s) for grafting. A fall in the hemoglobin from normal preoperative levels (e.g. 15) to postoperative levels of 6 to 10 are inevitable. There is no benefit from transfusions until the hemoglobin falls below 7.5.[26] Institutions should establish protocols to ensure transfusions are not given unless the hemoglobin falls below 7.5 without some additional compelling reason(s).[27]
- Delayed healing or refracture of sternum - the sternum is bifurcated longitudinally (a median sternotomy) and retracted to access the heart. Failure to follow "sternal precautions" following surgery could result in delayed healing or refracture of the sternum which was sutured at the closure of the chest wound:
- Hold a pillow against the chest whenever getting out of or into a chair or bed; or coughing, sneezing, blowing nose, or laughing, in order to oppose the intrathoracic outward force created by these activities on the healing sternum.
- Avoid using the pectoral muscles, such as by pushing on the chair arms to assist one's self out of a chair, or by using the arms to assist in sitting down. Proper standing technique is to rock three times in the chair and then stand to provide momentum for moving the center of gravity from the sitting to the standing position. Proper sitting technique is to slowly lower the bottom toward the chair seat using gluteus and quadriceps muscles ("legs only") without grabbing the chair arms. Second, patients should avoid lifting objects utilizing the pectoral muscles: carrying light objects with arms extended down at sides, and lifting light objects with the elbows pressed to the chest and using the biceps, are acceptable. Also, avoid using the arms overhead.
- Avoid sitting in the car front seat (no driving) for at least four weeks: the explosion of the deployment of an airbag could refracture the sternal union.
General surgery associated
- Infection at incision sites
- Sepsis
- Deep vein thrombosis
- Anesthetic complications such as malignant hyperthermia
- Keloid scarring
- Chronic pain at incision sites
- Chronic stress related illnesses
Procedure
- The patient is brought to the operating room and moved onto the operating table.
- An anaesthetist places intravenous and arterial lines and injects an analgesic, usually fentanyl, intravenously, followed within minutes by an induction agent (usually propofol or etomidate) to render the patient unconscious.
- An endotracheal tube is inserted and secured by the anaesthetist and mechanical ventilation is started. General anaesthesia is maintained with an inhaled volatile anesthetic agent such as isoflurane.
- The chest is opened via a median sternotomy and the heart is examined by the surgeon.
- The bypass grafts are harvested – frequent vessels are the internal thoracic arteries, radial arteries and saphenous veins. When harvesting is done, the patient is given heparin to inhibit blood clotting.
- In the case of "off-pump" surgery, the surgeon places devices to stabilize the heart.
- In the case of "on-pump" surgery, the surgeon sutures cannulae into the heart and instructs the perfusionist to start cardiopulmonary bypass (CPB) normally instructing the perfusionist to "Go on pump". Once CPB is established, there are two technical approaches: either the surgeon places the aortic cross-clamp across the aorta and instructs the perfusionist to deliver cardioplegia with a cooled potassium mixture to stop the heart and slow its metabolism or performing bypasses on beating state (on-pump beating).
- One end of each vein graft is sewn on to the coronary arteries beyond the obstruction and the other end is attached to the aorta or one of its branches. For the internal thoracic artery, the artery is severed and the proximal intact artery is sewn to the LAD beyond the obstruction. Aside the latter classical approach, there are emerging techniques for construction of composite grafts as to avoiding connecting grafts on the ascending aorta (Un-Aortic) in view of decreasing neurologic complications.
- The heart is restarted by removing the aortic cross clamp; or in "off-pump" surgery, the stabilizing devices are removed. In cases where the aorta is partially occluded by a C-shaped clamp, the heart is restarted and suturing of the grafts to the aorta is done in this partially occluded section of the aorta while the heart is beating.
- Once the grafts are completed distally and proximally, the patient is rewarmed to a normal temperature and the heart and other pressures are normal to support coming off the bypass machine, weaning off the bypass machine begins.
- The perfusionist makes sure they have enough volume to come off bypass, confirms that anesthesia is ventilating the patient, confirms that vacuum assist is off (if used), and vocalizes each step in the weaning process to the surgeon and anesthesia. Volume can be given to the patient through the arterial line of the bypass machine while the aortic cannula is still in.
- Protamine is given to reverse the effects of heparin.
- Chest tubes are placed in the mediastinal and pleural space to drain blood from around the heart and lungs.
- The sternum is wired together and the incisions are sutured closed.
- The patient is moved to an intensive care unit (ICU) or cardiac universal bed (CUB) to recover. Nurses in the ICU monitor blood pressure, urine output, respiratory status, and chest tubes for excessive or no drainage.
- After awakening and stabilizing in the ICU for 18 to 24 hours, the person is transferred to the cardiac surgery ward. If the patient is in a CUB, equipment and nursing is "stepped down" appropriate to the patient's progress without having to move the patient. Vital sign monitoring, remote rhythm monitoring, early ambulation with assistance, breathing exercises, pain control, blood sugar monitoring with intravenous insulin administration by protocol, and anti-platelet agents are all standards of care.
- The patient without complications is discharged in four or five days.
Minimally invasive technique
Alternate methods of minimally invasive coronary artery bypass surgery have been developed. Off-pump coronary artery bypass (OPCAB) is a technique of performing bypass surgery without the use of cardiopulmonary bypass (the heart-lung machine).[28] Avoidance of aortic manipulation may be achieved through the "anaortic" or no-touch OPCAB technique, which has been shown to reduce stroke and mortality compared to on-pump CABG.[29] Further refinements to OPCAB have resulted in minimally invasive direct coronary artery bypass surgery (MIDCAB), a technique of performing bypass surgery through a 5 to 10 cm incision.[30]
Hybrid Coronary Revascualrisation, where the LIMA-to-LAD anastomosis is combined with percutaneous stents in other atherosclerotic sites, has been shown to have significant advantages compared to conventional CABG, including a decrease in the incidence of blood transfusion, and a reduced intubation time. A 2018 meta-analysis has however demonstrated a greater financial cost when compared to conventional CABG.[31]
Choice of source of grafts

The choice of vessel(s) is highly dependent upon the particular surgeon and institution. Typically, the left internal thoracic artery (LITA) (previously referred to as left internal mammary artery or LIMA) is grafted to the left anterior descending artery and a combination of other arteries and veins is used for other coronary arteries.[32] The great saphenous vein from the leg is used approximately in 80% of all grafts for CABG.[33] The right internal thoracic (mammary) artery (RITA or RIMA) and the radial artery from the forearm are frequently used as well; in the U.S., these vessels are usually harvested either endoscopically, using a technique known as endoscopic vessel harvesting (EVH), or with the open-bridging technique, employing two or three small incisions. The right gastroepiploic artery from the stomach is infrequently used given the difficult mobilization from the abdomen.
Follow up
- Acute - patients without complications are typically seen 3–4 weeks post operatively, at which time driving may be resumed and formal cardiac rehabilitation begun to increase aerobic endurance and muscular strength.
- Chronic -
- a cardiac stress test at five years is recommended, even in the absence of cardiac symptoms.[34][35]
- an intensive medical regimen including statins, aspirin, and aerobic exercise is essential to delaying the progression of plaque formation in both the native and grafted vessels.
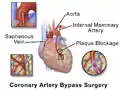 Illustration depicting coronary artery bypass surgery (double bypass)
Illustration depicting coronary artery bypass surgery (double bypass) Illustration of Single bypass
Illustration of Single bypass Illustration of Double bypass
Illustration of Double bypass Illustration of Triple bypass
Illustration of Triple bypass Illustration of Quadruple bypass
Illustration of Quadruple bypass
Number performed
CABG is one of the most common procedures performed during U.S. hospital stays; it accounted for 1.4% of all operating room procedures performed in 2011.[36] Between 2001 and 2011, however, its volume decreased by 46%, from 395,000 operating procedures performed in 2001 to 213,700 procedures in 2011.[37]
Between 2000 and 2012, the number of CABG procedures carried out decreased across the majority of OECD countries. However, there remained substantial variation in the rate of procedures, with the U.S. carrying out four times as many CABG operations per 100,000 people as Spain.[38] These differences do not appear to be closely related to the incidence of heart disease, but may be due to variation in financial resources, capacity, treatment protocols and reporting methods.[39]
History
- The first coronary artery bypass surgery was performed in the United States on May 2, 1960, at the Albert Einstein College of Medicine-Bronx Municipal Hospital Center by a team led by Robert H. Goetz and the thoracic surgeon, Michael Rohman with the assistance of Jordan Haller and Ronald Dee.[40][41] In this technique the vessels are held together with circumferential ligatures over an inserted metal ring. The internal mammary artery was used as the donor vessel and was anastomosed to the right coronary artery. The actual anastomosis with the Rosenbach ring took fifteen seconds and did not require cardiopulmonary bypass. The disadvantage of using the internal mammary artery was that, at autopsy nine months later, the anastomosis was open, but an atheromatous plaque had occluded the origin of the internal mammary that was used for the bypass.
- Soviet cardiac surgeon, Vasilii Kolesov, performed the first successful internal mammary artery–coronary artery anastomosis in 1964.[42][43] However, Goetz has been cited by others, including Kolesov,[44] as the first successful human coronary artery bypass.[45][46][47][48][49][50] Goetz's case has frequently been overlooked. Confusion has persisted for over 40 years and seems to be due to the absence of a full report and to misunderstanding about the type of anastomosis that was created. The anastomosis was intima-to-intima, with the vessels held together with circumferential ligatures over a specially designed metal ring. Kolesov did the first successful coronary bypass using a standard suture technique in 1964, and over the next five years he performed 33 sutured and mechanically stapled anastomoses in Leningrad (now St. Petersburg), USSR.[51][52]
- René Favaloro, an Argentine surgeon, achieved a physiologic approach in the surgical management of coronary artery disease—the bypass grafting procedure—at the Cleveland Clinic in May 1967.[43][53] His new technique used a saphenous vein autograft to replace a stenotic segment of the right coronary artery. Later, he successfully used the saphenous vein as a bypassing channel, which has become the typical bypass graft technique we know today; in the U.S., this vessel is typically harvested endoscopically, using a technique known as endoscopic vessel harvesting (EVH).
- Soon Dudley Johnson extended the bypass to include left coronary arterial systems.[43]
- In 1968, doctors Charles Bailey, Teruo Hirose and George Green used the internal mammary artery instead of the saphenous vein for the grafting.[43]
Cost
According to the CDC, the average cost of hospitalization (only) associated with a coronary bypass operation in the United States in 2013 was $38,707, for an aggregate hospitalization cost of $6.4 billion.[54] The International Federation of Healthcare Plans[55] has estimated the average cost of hospitalization and physician fees for a coronary bypass operation in various countries as shown in the Table below.[56]
| Country | Cost |
|---|---|
| United States | $75,345 |
| Australia | $42,130 |
| New Zealand | $40,368 |
| Switzerland | $36,509 |
| Argentina | $16,492 |
| Spain | $16,247 |
| Netherlands | $15,742 |
| India | $1,583[57] |
See also
References
- "Bypass Surgery, Coronary Artery". American Heart Association. Retrieved March 26, 2010.
- "Results for "aortocoronary bypass,coronary artery bypass graft" between 1960 and 2008". Google Ngram Viewer. Retrieved 8 January 2015.
- Eagle KA, Guyton RA, Davidoff R, Edwards FH, Ewy GA, Gardner TJ, et al. (October 2004). "ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery)". Circulation. 110 (14): e340-437. doi:10.1161/01.CIR.0000138790.14877.7D. PMID 15466654. S2CID 37717092.
- Kolata, Gina. "New Heart Studies Question the Value Of Opening Arteries" The New York Times, March 21, 2004. Retrieved January 14, 2011.
- Ohki S, Kaneko T, Satoh Y, Inaba H, Kaki N, Yamagishi T, Morishita Y (September 2002). "[Coronary artery bypass grafting in octogenarian]". Kyobu Geka. The Japanese Journal of Thoracic Surgery (in Japanese). 55 (10): 829–33, discussion 833–6. PMID 12233100.
- Weintraub WS, Clements SD, Crisco LV, Guyton RA, Craver JM, Jones EL, Hatcher CR (March 2003). "Twenty-year survival after coronary artery surgery: an institutional perspective from Emory University". Circulation. 107 (9): 1271–7. doi:10.1161/01.CIR.0000053642.34528.D9. PMID 12628947.
- Kitamura S, Kawachi K, Kawata T, Kobayashi S, Mizuguchi K, Kameda Y, et al. (March 1996). "[Ten-year survival and cardiac event-free rates in Japanese patients with the left anterior descending artery revascularized with internal thoracic artery or saphenous vein graft: a comparative study]". Nihon Geka Gakkai Zasshi (in Japanese). 97 (3): 202–9. PMID 8649330.
- Arima M, Kanoh T, Suzuki T, Kuremoto K, Tanimoto K, Oigawa T, Matsuda S (August 2005). "Serial angiographic follow-up beyond 10 years after coronary artery bypass grafting". Circulation Journal. 69 (8): 896–902. doi:10.1253/circj.69.896. PMID 16041156.
- Rihal CS, Raco DL, Gersh BJ, Yusuf S (November 2003). "Indications for coronary artery bypass surgery and percutaneous coronary intervention in chronic stable angina: review of the evidence and methodological considerations". Circulation. 108 (20): 2439–45. doi:10.1161/01.CIR.0000094405.21583.7C. PMID 14623791.
- SoS Investigators (September 2002). "Coronary artery bypass surgery versus percutaneous coronary intervention with stent implantation in patients with multivessel coronary artery disease (the Stent or Surgery trial): a randomised controlled trial". Lancet. 360 (9338): 965–70. doi:10.1016/S0140-6736(02)11078-6. PMID 12383664. S2CID 45372972.
- Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. (March 2009). "Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease". The New England Journal of Medicine. 360 (10): 961–72. doi:10.1056/NEJMoa0804626. hdl:2437/95138. PMID 19228612.
- Desai ND (January 2008). "Pitfalls assessing the role of drug-eluting stents in multivessel coronary disease". The Annals of Thoracic Surgery. 85 (1): 25–7. doi:10.1016/j.athoracsur.2007.08.063. PMID 18154771.
- Hannan EL, Wu C, Walford G, Culliford AT, Gold JP, Smith CR, et al. (January 2008). "Drug-eluting stents vs. coronary-artery bypass grafting in multivessel coronary disease". The New England Journal of Medicine. 358 (4): 331–41. doi:10.1056/NEJMoa071804. PMID 18216353. S2CID 8979667.
- Li X, Kong M, Jiang D, Dong A (March 2014). "Comparing coronary artery bypass grafting with drug-eluting stenting in patients with diabetes mellitus and multivessel coronary artery disease: a meta-analysis". Interactive Cardiovascular and Thoracic Surgery. 18 (3): 347–54. doi:10.1093/icvts/ivt509. PMC 3930218. PMID 24345688.
- Reynolds Reynolds AC, King N (August 2018). "Hybrid coronary revascularization versus conventional coronary artery bypass grafting: Systematic review and meta-analysis". Medicine. 97 (33): e11941. doi:10.1097/MD.0000000000011941. PMC 6112891. PMID 30113498.
- Harmon K (August 6, 2009). "Heart-Lung Machine May Not Be the Culprit in Post-Op "Pump Head" Syndrome". ScientificAmerican.com. Retrieved February 2, 2010.
- Selnes OA, Gottesman RF, Grega MA, Baumgartner WA, Zeger SL, McKhann GM (January 2012). "Cognitive and neurologic outcomes after coronary-artery bypass surgery". The New England Journal of Medicine. 366 (3): 250–7. doi:10.1056/NEJMra1100109. PMID 22256807. S2CID 2094158.
- Stutz, Bruce "Pumphead: Does the heart-lung machine have a dark side?" Scientific American, January 9, 2009.
- Li AE, Fishman EK (October 2003). "Evaluation of complications after sternotomy using single- and multidetector CT with three-dimensional volume rendering". AJR. American Journal of Roentgenology. 181 (4): 1065–70. doi:10.2214/ajr.181.4.1811065. PMID 14500232.
- Benstoem C, Stoppe C, Liakopoulos OJ, Ney J, Hasenclever D, Meybohm P, Goetzenich A (May 2017). Cochrane Heart Group (ed.). "Remote ischaemic preconditioning for coronary artery bypass grafting (with or without valve surgery)". The Cochrane Database of Systematic Reviews. 5: CD011719. doi:10.1002/14651858.CD011719.pub3. PMC 6481544. PMID 28475274.
- Force T, Hibberd P, Weeks G, Kemper AJ, Bloomfield P, Tow D, et al. (September 1990). "Perioperative myocardial infarction after coronary artery bypass surgery. Clinical significance and approach to risk stratification". Circulation. 82 (3): 903–12. doi:10.1161/01.CIR.82.3.903. PMID 2394010.
- Bucerius J, Gummert JF, Walther T, Schmitt DV, Doll N, Falk V, Mohr FW (April 2004). "On-pump versus off-pump coronary artery bypass grafting: impact on postoperative renal failure requiring renal replacement therapy". The Annals of Thoracic Surgery. 77 (4): 1250–6. doi:10.1016/S0003-4975(03)01346-8. PMID 15063246.
- Silber JH, Rosenbaum PR, Schwartz JS, Ross RN, Williams SV (July 1995). "Evaluation of the complication rate as a measure of quality of care in coronary artery bypass graft surgery". JAMA. 274 (4): 317–23. doi:10.1001/jama.1995.03530040045039. PMID 7609261.
- Selnes OA, Gottesman RF, Grega MA, Baumgartner WA, Zeger SL, McKhann GM (January 2012). "Cognitive and neurologic outcomes after coronary-artery bypass surgery". The New England Journal of Medicine. 366 (3): 250–7. doi:10.1056/NEJMra1100109. PMID 22256807. S2CID 2094158.
- Leitch JW, Thomson D, Baird DK, Harris PJ (September 1990). "The importance of age as a predictor of atrial fibrillation and flutter after coronary artery bypass grafting". The Journal of Thoracic and Cardiovascular Surgery. 100 (3): 338–42. doi:10.1016/S0022-5223(19)35525-4. PMID 2391970.
- Murphy GJ, Pike K, Rogers CA, Wordsworth S, Stokes EA, Angelini GD, Reeves BC (March 2015). "Liberal or restrictive transfusion after cardiac surgery" (PDF). The New England Journal of Medicine. 372 (11): 997–1008. doi:10.1056/NEJMoa1403612. hdl:2381/36005. PMID 25760354.
- Spertus J (March 2015). ""TITRe"ing the approach to transfusions after cardiac surgery". The New England Journal of Medicine. 372 (11): 1069–70. doi:10.1056/NEJMe1415394. PMID 25760360. S2CID 205078998.
- Sabik J (2010). "Off Pump Bypass Surgery: Improving outcomes for coronary artery bypass surgery". Clevelandclinic.com. Retrieved February 28, 2011.
- Zhao DF, Edelman JJ, Seco M, Bannon PG, Wilson MK, Byrom MJ, et al. (February 2017). "Coronary Artery Bypass Grafting With and Without Manipulation of the Ascending Aorta: A Network Meta-Analysis". Journal of the American College of Cardiology. 69 (8): 924–936. doi:10.1016/j.jacc.2016.11.071. PMID 28231944.
- Sabik J (2010). "Minimally Invasive Bypass Surgery". Clevelandclinic.com. Retrieved February 28, 2011.
- Reynolds AC, King N (August 2018). "Hybrid coronary revascularization versus conventional coronary artery bypass grafting: Systematic review and meta-analysis". Medicine. 97 (33): e11941. doi:10.1097/MD.0000000000011941. PMC 6112891. PMID 30113498.
- Head SJ, Milojevic M, Taggart DP, Puskas JD (October 2017). "Current Practice of State-of-the-Art Surgical Coronary Revascularization". Circulation. 136 (14): 1331–1345. doi:10.1161/CIRCULATIONAHA.116.022572. PMID 28972063. S2CID 19567089.
- Mawhinney JA, Mounsey CA, Taggart DP (June 2018). "The potential role of external venous supports in coronary artery bypass graft surgery". European Journal of Cardio-Thoracic Surgery. 53 (6): 1127–1134. doi:10.1093/ejcts/ezx432. PMID 29228235.
- American College of Cardiology. "Five Things Physicians and Patients Should Question" (PDF). Choosing Wisely: An Initiative of the ABIM Foundation. Archived from the original (PDF) on June 24, 2012. Retrieved August 17, 2012.
- Douglas PS, Garcia MJ, Haines DE, Lai WW, Manning WJ, Patel AR, et al. (March 2011). "ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 Appropriate Use Criteria for Echocardiography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance Endorsed by the American College of Chest Physicians". Journal of the American College of Cardiology. 57 (9): 1126–66. doi:10.1016/j.jacc.2010.11.002. PMID 21349406.
- Weiss AJ, Elixhauser A, Andrews RM (February 2014). "Characteristics of Operating Room Procedures in U.S. Hospitals, 2011". HCUP Statistical Brief #170. Rockville, MD: Agency for Healthcare Research and Quality.
- Weiss AJ, Elixhauser A (March 2014). "Trends in Operating Room Procedures in U.S. Hospitals, 2001—2011". HCUP Statistical Brief #171. Rockville, MD: Agency for Healthcare Research and Quality.
- "Indicator: International comparisons of surgical procedures". QualityWatch. Nuffield Trust & Health Foundation. Archived from the original on 22 July 2015. Retrieved 5 May 2015.
- Lafortune, Gaetan. "Comparing activities and performance of the hospital sector in Europe: how many surgical procedures performed as inpatient and day cases?" (PDF). OECD. OECD. Retrieved 5 May 2015.
- Dee R (2003). "Who assisted whom?". Texas Heart Institute Journal. 30 (1): 90. PMC 152850. PMID 12638685.
- Haller JD, Olearchyk AS (2002). "Cardiology's 10 greatest discoveries". Texas Heart Institute Journal. 29 (4): 342–4. PMC 140304. PMID 12484626.
- Kolessov VI (October 1967). "Mammary artery-coronary artery anastomosis as method of treatment for angina pectoris". The Journal of Thoracic and Cardiovascular Surgery. 54 (4): 535–44. doi:10.1016/s0022-5223(19)43061-4. PMID 6051440.
- Mehta NJ, Khan IA (2002). "Cardiology's 10 greatest discoveries of the 20th century". Texas Heart Institute Journal. 29 (3): 164–71. PMC 124754. PMID 12224718.
- Kolesov VI, Potashov LV (1965). "[Surgery of coronary arteries]". Eksperimental'naia Khirurgiia I Anesteziologiia (in Russian). 10 (2): 3–8. PMID 5851057.
- Olearchyk, AS (1988). "Coronary revascularization: past, present and future". J Ukr Med Assoc North Am. 1 (117): 3–34.
- Olearchyk AS, Olearchyk RM (January 1999). "Reminiscences of Vasilii I. Kolesov". The Annals of Thoracic Surgery. 67 (1): 273–6. doi:10.1016/S0003-4975(98)01225-9. PMID 10086577.
- Glenn WW (April 1972). "Some reflections on the coronary bypass operation". Circulation. 45 (4): 869–77. doi:10.1161/01.CIR.45.4.869. PMID 5016019.
- Ochsner JL, Mills NL (1978). Coronary artery surgery. Philadelphia: Lea & Febiger.
- Cushing WJ, Magovern GJ, Olearchyk AS (November 1986). "Internal mammary artery graft: retrospective report with 17 years' survival". The Journal of Thoracic and Cardiovascular Surgery. 92 (5): 963–4. doi:10.1016/S0022-5223(19)35860-X. PMID 3773554.
- Konstantinov IE (June 2000). "Robert H. Goetz: the surgeon who performed the first successful clinical coronary artery bypass operation". The Annals of Thoracic Surgery. 69 (6): 1966–72. doi:10.1016/S0003-4975(00)01264-9. PMID 10892969.
- Kolesov VI, Kolesov EV (February 1991). "Twenty years' results with internal thoracic artery-coronary artery anastomosis". The Journal of Thoracic and Cardiovascular Surgery. 101 (2): 360–1. doi:10.1016/S0022-5223(19)36773-X. PMID 1992247.
- Haller JD, Olearchyk AS (2002). "Cardiology's 10 greatest discoveries". Texas Heart Institute Journal. 29 (4): 342–4. PMC 140304. PMID 12484626.
Reference 4
- Favaloro RG, Effler DB, Cheanvechai C, Quint RA, Sones FM (November 1971). "Acute coronary insufficiency (impending myocardial infarction and myocardial infarction): surgical treatment by the saphenous vein graft technique". The American Journal of Cardiology. 28 (5): 598–607. doi:10.1016/0002-9149(71)90104-4. PMID 5116978.
- "www.cdc.gov" (PDF).
- "About IFHP — IFHP".
- "static.squarespace.com" (PDF). Archived from the original (PDF) on 2014-12-16.
- Gokhale K (July 28, 2013). "Heart Surgery in India for ,583 Costs $106,385 in U.S". Bloomberg.