Eplerenone
Eplerenone, sold under the brand name Inspra, is a steroidal antimineralocorticoid of the spirolactone group that is used as an adjunct in the management of chronic heart failure and high blood pressure, particularly for patients with resistant hypertension due to elevated aldosterone. Classed as a selective aldosterone receptor antagonist (SARA),[5] it is similar to the diuretic spironolactone, though it is much more selective for the mineralocorticoid receptor in comparison (i.e., does not possess any antiandrogen, progestogen, glucocorticoid, or estrogenic effects), and is specifically marketed for reducing cardiovascular risk in patients following myocardial infarction. Eplerenone is a potassium-sparing diuretic, meaning that it helps the body get rid of water but still keep potassium.
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ɛpˈlɛrənoʊn/ |
| Trade names | Inspra, Epnone, Dosterep |
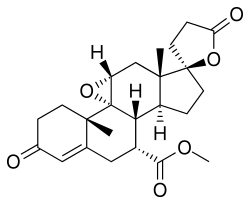
| Other names | SC-66110; CGP-30083; 9-11α-Epoxymexrenone; 9,11α-Epoxy-7α-methoxycarbonyl-3-oxo-17α-pregn-4-ene-21,17-carbolactone |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a603004 |
| Pregnancy category |
|
| Routes of administration | By mouth (tablets) |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | ~70%[1] |
| Protein binding | ~50% (33–60%) (primarily to α1-acid glycoprotein)[1][2] |
| Metabolism | Liver (CYP3A4)[1][2] |
| Metabolites | 6β-OH-EPL, 6β,21-OH-EPL, 21-OH-EPL, 3α,6β-OH-EPL[1] (All inactive)[1] |
| Elimination half-life | 4–6 hours[3] |
| Excretion | Urine (67%), feces (32%)[4] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.106.615 |
| Chemical and physical data | |
| Formula | C24H30O6 |
| Molar mass | 414.498 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
It was patented in 1983 and approved for medical use in the United States in 2002.[6][7] Eplerenone is currently approved for sale in Canada, the US, EU, Netherlands and Japan.[7] Eplerenone costs an estimated $2.93 per day when treating congestive heart failure and $5.86 per day when treating hypertension.[8]
Medical uses
Heart failure
Eplerenone is specifically indicated for the reduction of risk of cardiovascular death in people with heart failure and left ventricular dysfunction within 3–14 days of an acute myocardial infarction, in combination with standard therapies and as treatment against hypertension. A variant of the spirolactone group, eplerenone was developed to counteract the depletion of essential potassium and magnesium levels that are common amongst other mineralocorticoid receptor antagonists.[9] It is a more expensive alternative to spironolactone.[10]
| Parameter | RALES | EPHESUS |
|---|---|---|
| Drug: | Spironolactone | Eplerenone |
| Patients enrolled (n) | 1663 | 6632 |
| Population/Inclusion Criteria | NYHA Class III at the time of Enrollment | NYHA Class I-IV |
| Target Dose | 50 mg/d | 50 mg/d |
| Mean Dose Achieved | 26 mg/d | 43.5 mg/d |
| Mean duration of follow-up | 24 mo | 16 mo |
| Diuretic | 100% | 60% |
Hypertension
Eplerenone can be used individually or in combination with other medications to treat hypertension.[3] In an 8-week trial with 417 patients with mild to moderate hypertension, eplerenone decreased systolic and diastolic blood pressure in a dose-dependent manner.[11] However, A 2017 Cochrane systematic review on eplerenone did not find any clinically important dose response in decreasing blood pressure for doses 50 to 400 mg daily. According to their meta-analysis, eplerenone lowered systolic blood pressure by 9.21 mmHg and diastolic blood pressure by 4.18 mmHg in people with primary hypertension.[12] Eplerenone effectively reduces blood pressure compared to agents such as spironolactone, enalapril, losartan and amlodipine, but its effect on mortality is still generally unknown.[11]
For persons with resistant hypertension, aldosterone antagonists (including eplerenone) were safe and in comparative studies reduced systolic blood pressure by 24 mm Hg and diastolic blood pressure by about 8 mm Hg.[13] Specifically, eplerenone is likely to be particularly effective in persons with resistant hypertension due to hyperaldosteronism, as indicated by a high blood plasma aldosterone and a low plasma renin activity.[14]
Central serous retinopathy
Eplerenone is being explored as a treatment for central serous retinopathy.[15] It is expected that as an antimineralocorticoid, eplerenone can inhibit over-activation of the mineralocorticoid receptor pathway in the choroid. The most recent clinical trial showed that eplerenone had no significant effect on chronic CSR.[16][17]
Other uses
Eplerenone, in contrast to spironolactone, does not have antiandrogenic effects, and hence is not useful in feminizing hormone therapy for transgender women and related indications.[18]
Contraindications
Eplerenone is contraindicated in patients with hyperkalaemia, severe renal impairment (creatinine Cl less than 30 ml/min), or severe hepatic impairment (Child-Pugh score C). The manufacturer of eplerenone also contraindicates ( relative C.I. ) concomitant treatment with ketoconazole, itraconazole or other potassium-sparing diuretics (though the manufacturer still considers taking these drugs to be absolute C.I.) Potential benefits should be weighted against possible risks.
Side effects
Adverse effects of aldosterone occur in the heart and brain, due to changes in water retention and excretion of sodium and potassium.[3] Common adverse drug reactions (ADRs) associated with the use of eplerenone include: hyperkalaemia, hypotension, dizziness, altered renal function, and increased creatinine concentration.[19] Eplerenone may have a lower incidence than spironolactone of sexual side effects such as feminization, gynecomastia, impotence, low sex drive and reduction of size of male genitalia.[8] This is because other antimineralocorticoids have structural elements of the progesterone molecule, causing progestogenic and antiandrogenic outcomes.[3] When considering taking these medicines, it is important to note the variations in their ability to offset the nongenomic effects of aldosterone.[3]
Currently, there is not enough evidence available from the randomized controlled trials on side effects of eplerenone to do a benefit versus risk assessment in people with primary hypertension. [20]
Interactions
Eplerenone is primarily metabolized by the cytochrome P450 enzyme CYP3A4. Thus the potential exists for adverse drug interactions with other drugs that induce or inhibit CYP3A4. Specifically, the concomitant use of the CYP3A4 potent inhibitors ketoconazole and itraconazole is contraindicated. Other CYP3A4 inhibitors including erythromycin, saquinavir, and verapamil should be used with caution. Other drugs that increase potassium concentrations may increase the risk of hyperkalemia associated with eplerenone therapy, including salt substitutes,[21] potassium supplements and other potassium-sparing diuretics.
Pharmacology
Eplerenone is an antimineralocorticoid, or an antagonist of the mineralocorticoid receptor (MR).[22] Eplerenone is also known chemically as 9,11α-epoxy-7α-methoxycarbonyl-3-oxo-17α-pregn-4-ene-21,17-carbolactone and "was derived from spironolactone by the introduction of a 9α,11α-epoxy bridge and by substitution of the 17α-thoacetyl group of spironolactone with a carbomethoxy group."[11] The drug controls high blood pressure by blocking the binding of aldosterone to the mineralocorticoid receptor (MR) in epithelial tissues, such as the kidney.[3] Blocking the action of aldosterone decreases blood volume and lowers blood pressure.[7] It has 10- to 20-fold lower affinity for the MR relative to spironolactone,[22] and is less potent in vivo as an antimineralocorticoid.[3] However, in contrast to spironolactone, eplerenone has little affinity for the androgen, progesterone, and glucocorticoid receptors.[22][3] It also has more consistently observed non-genomic antimineralocorticoid effects relative to spironolactone (see membrane mineralocorticoid receptor).[3] Eplerenone differs from spironolactone in its extensive metabolism, with a short half-life and inactive metabolites.[3]
Eplerenone seems to be about 50 to 75% as potent as spironolactone as an antimineralocorticoid.[23] Hence, 25 mg/day spironolactone may be equivalent to approximately 50 mg/day eplerenone.[24]
See also
References
- Lemke TL, Williams DA (24 January 2012). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 743–. ISBN 978-1-60913-345-0.
- Sica DA (January 2005). "Pharmacokinetics and pharmacodynamics of mineralocorticoid blocking agents and their effects on potassium homeostasis". Heart Failure Reviews. 10 (1): 23–9. doi:10.1007/s10741-005-2345-1. PMID 15947888. S2CID 21437788.
- Struthers A, Krum H, Williams GH (April 2008). "A comparison of the aldosterone-blocking agents eplerenone and spironolactone". Clinical Cardiology. 31 (4): 153–8. doi:10.1002/clc.20324. PMC 6652937. PMID 18404673.
- Frishman WH, Cheng-Lai A, Nawarskas J (4 January 2005). Current Cardiovascular Drugs. Springer Science & Business Media. pp. 246–. ISBN 978-1-57340-221-7.
- Delyani JA, Rocha R, Cook CS, Tobert DS, Levin S, Roniker B, et al. (2001). "Eplerenone: a selective aldosterone receptor antagonist (SARA)". Cardiovascular Drug Reviews. 19 (3): 185–200. doi:10.1111/j.1527-3466.2001.tb00064.x. PMID 11607037.
- Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 459. ISBN 9783527607495.
- "Inspra (Eplerenone)". Drug Development Technology. Retrieved 2016-04-19.
- Craft J (April 2004). "Eplerenone (Inspra), a new aldosterone antagonist for the treatment of systemic hypertension and heart failure". Proceedings. 17 (2): 217–20. doi:10.1080/08998280.2004.11927973. PMC 1200656. PMID 16200104.
- Montalescot G, Pitt B, Lopez de Sa E, Hamm CW, Flather M, Verheugt F, et al. (September 2014). "Early eplerenone treatment in patients with acute ST-elevation myocardial infarction without heart failure: the Randomized Double-Blind Reminder Study". European Heart Journal. 35 (34): 2295–302. doi:10.1093/eurheartj/ehu164. PMID 24780614.
- Chatterjee S, Moeller C, Shah N, Bolorunduro O, Lichstein E, Moskovits N, Mukherjee D (August 2012). "Eplerenone is not superior to older and less expensive aldosterone antagonists". The American Journal of Medicine. 125 (8): 817–25. doi:10.1016/j.amjmed.2011.12.018. PMID 22840667.
- Brown NJ (May 2003). "Eplerenone: cardiovascular protection". Circulation. 107 (19): 2512–8. doi:10.1161/01.CIR.0000071081.35693.9A. PMID 12756192.
- Tam TS, Wu MH, Masson SC, Tsang MP, Stabler SN, Kinkade A, et al. (February 2017). "Eplerenone for hypertension". The Cochrane Database of Systematic Reviews. 2: CD008996. doi:10.1002/14651858.CD008996.pub2. PMC 6464701. PMID 28245343.
- Dahal K, Kunwar S, Rijal J, Alqatahni F, Panta R, Ishak N, Russell RP (November 2015). "The Effects of Aldosterone Antagonists in Patients With Resistant Hypertension: A Meta-Analysis of Randomized and Nonrandomized Studies". American Journal of Hypertension. 28 (11): 1376–85. doi:10.1093/ajh/hpv031. PMID 25801902.
- Spence JD (May 2017). "Rational Medical Therapy Is the Key to Effective Cardiovascular Disease Prevention". The Canadian Journal of Cardiology. 33 (5): 626–634. doi:10.1016/j.cjca.2017.01.003. PMID 28449833.
- Salehi M, Wenick AS, Law HA, Evans JR, Gehlbach P (December 2015). "Interventions for central serous chorioretinopathy: a network meta-analysis". The Cochrane Database of Systematic Reviews (12): CD011841. doi:10.1002/14651858.CD011841.pub2. PMC 5030073. PMID 26691378.
- Lotery, Andrew (25 January 2020). "Eplerenone for chronic central serous chorioretinopathy in patients with active, previously untreated disease for more than 4 months (VICI): a randomised, double-blind, placebo-controlled trial". The Lancet. 395 (10220): 294–303. doi:10.1016/S0140-6736(19)32981-2. PMID 31982075.
- Trials Centre, Bristol. "VICI Trial YouTube video". Twitter.
- Bass M, Gonzalez LJ, Colip L, Sharon N, Conklin J (November 2018). "Rethinking gender: The nonbinary approach". American Journal of Health-System Pharmacy. 75 (22): 1821–1823. doi:10.2146/ajhp180236. PMID 30228164.
- Rossi S (2006). Australian Medicines Handbook 2006. Australian Medicines Handbook. ISBN 978-0-9757919-2-9.
- Tam TS, Wu MH, Masson SC, Tsang MP, Stabler SN, Kinkade A, et al. (February 2017). "Eplerenone for hypertension". The Cochrane Database of Systematic Reviews. 2: CD008996. doi:10.1002/14651858.CD008996.pub2. PMC 6464701. PMID 28245343.
- LoSalt Advisory Statement (PDF)
- Delyani JA (April 2000). "Mineralocorticoid receptor antagonists: the evolution of utility and pharmacology". Kidney International. 57 (4): 1408–11. doi:10.1046/j.1523-1755.2000.00983.x. PMID 10760075.
- Struthers A, Krum H, Williams GH (April 2008). "A comparison of the aldosterone-blocking agents eplerenone and spironolactone". Clin Cardiol. 31 (4): 153–8. doi:10.1002/clc.20324. PMC 6652937. PMID 18404673.
- Peter L. Thompson (28 January 2011). Coronary Care Manual. Elsevier Health Sciences. pp. 254–. ISBN 0-7295-7927-1.