Human herpesvirus 6
Human herpesvirus 6 (HHV-6) is the common collective name for human betaherpesvirus 6A (HHV-6A) and human betaherpesvirus 6B (HHV-6B). These closely related viruses are two of the nine herpesviruses known to have humans as their primary host.[1]
| Human herpesvirus 6 | |
|---|---|
.jpg.webp) | |
| Electron micrograph of one of the HHV6 species | |
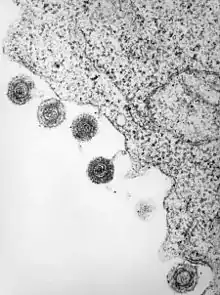 | |
| HHV-6 released from a lymphocyte which has been infected | |
| Scientific classification | |
| (unranked): | Virus |
| Realm: | Duplodnaviria |
| Kingdom: | Heunggongvirae |
| Phylum: | Peploviricota |
| Class: | Herviviricetes |
| Order: | Herpesvirales |
| Family: | Herpesviridae |
| Subfamily: | Betaherpesvirinae |
| Genus: | Roseolovirus |
| Groups included | |
| Cladistically included but traditionally excluded taxa | |
|
All other Roseolovirus spp.: | |
HHV-6A and HHV-6B are double stranded DNA viruses within the Betaherpesvirinae subfamily and of the genus Roseolovirus. HHV-6A and HHV-6B infect almost all of the human populations that have been tested.[2]
HHV-6A has been described as more neurovirulent,[3] and as such is more frequently found in patients with neuroinflammatory diseases such as multiple sclerosis.[4] HHV-6 (and HHV-7) levels in the brain are also elevated in people with Alzheimer's disease.[5]
HHV-6B primary infection is the cause of the common childhood illness exanthema subitum (also known as roseola infantum or sixth disease). It is passed on from child to child. It is uncommon for adults to contract this disease as most everyone has had it by kindergarten, and once contracted, an antibody is formed help to prevent becoming reinfected in the future. Additionally, HHV-6B reactivation is common in transplant recipients, which can cause several clinical manifestations such as encephalitis, bone marrow suppression, and pneumonitis.[6]
A variety of tests are used in the detection HHV-6, some of which do not differentiate the two species.[7]
History

During 1986, Syed Zaki Salahuddin, Dharam Ablashi, and Robert Gallo cultivated peripheral blood mononuclear cells from patients with AIDS and lymphoproliferative illnesses. Short-lived, large, refractile cells that frequently contained intranuclear and/or intracytoplasmic inclusion bodies were documented. Electron microscopy revealed a novel virus that they named Human B-Lymphotrophic Virus (HBLV).[8][9]
Shortly after its discovery, Ablashi et al. described five cell lines that can be infected by the newly discovered HBLV. They published that HSB-2, a particular T-cell line, is highly susceptible to infection. Ablashi's pioneering research concluded by suggesting that the virus name be changed from HBLV to HHV-6, in accord with the published provisional classification of herpes viruses.[10][11]
Years later, HHV-6 was divided into subtypes. Early research (1992) described two very similar, yet unique variants: HHV-6A and HHV-6B. The distinction was warranted due to unique restriction endonuclease cleavages, monoclonal antibody reactions,[12] and growth patterns.[13]
HHV-6A includes several adult-derived strains and its disease spectrum is not well defined, although it is thought by some to be more neurovirulent.[14][15] HHV-6B is commonly detected in children with roseola infantum, as it is the etiologic agent for this condition. Within these two viruses is a sequence homology of 95%.[16]
In 2012, HHV-6A and HHV-6B were officially recognized as distinct species.[1]
Taxonomy
HHV-6A and HHV-6B were recognized by the International Committee on Taxonomy of Viruses (ICTV) as distinct species in 2012. Human Roseoloviruses include HHV-6A, HHV-6B and HHV-7.[1]
Herpesvirus was established as a genus in 1971 in the first report of the ICTV. This genus consisted of 23 viruses among 4 groups.[17] In 1976, a second ICTV report was released in which this genus was elevated to the family level — the herpetoviridae. Because of possible confusion with viruses derived from reptiles, the family name was changed in the third report (1979) to herpesviridae. In this report, the family Herpesviridae was divided into 3 subfamilies (alphaherpesvirinae, betaherpesvirinae and gammaherpesvirinae) and 5 unnamed genera; 21 viruses were recognized as members of the family.[18]
In 2009, the order Herpesvirales was created. This was necessitated by the discovery that the herpes viruses of fish and molluscs are only distantly related to those of birds and mammals. Order Herpesvirales contains three families, the Herpesviridae, which contains the long-recognized herpesviruses of mammals, birds, and reptiles, plus two new families — the family Alloherpesviridae which incorporates herpes viruses of bony fish and frogs, and the family Malacoherpesviridae which contains viruses of molluscs.[19]
As of 2012, this order currently has 3 families, 4 subfamilies (1 unassigned), 18 genera (4 unassigned) and 97 species.[1]
Structure
The diameter of an HHV-6 virion is about 2000 angstroms.[9] The virion's outer portion consists of a lipid bilayer membrane that contains viral glycoproteins and is derived from that of the host. Below this membrane envelope is a tegument which surrounds an icosahedral capsid, composed of 162 capsomeres. The protective capsid of HHV-6 contains double stranded linear DNA.
During maturation of HHV-6 virions, human cell membranes are used to form viral lipid envelopes (as is characteristic of all enveloped viruses). During this process HHV-6 utilizes lipid rafts, which are membranous microdomains enriched by cholesterol, sphingolipids, and glycosylphosphatidylinositol-anchored proteins.[20] Early researchers suspected that HHV-6 virions mature in the nucleus; some even incorrectly published this, as they generalized and applied to HHV-6 what was known about other viruses. However, researched published in 2009 suggests that the HHV-6 virus utilizes trans-Golgi-network-derived vesicles for assembly.[20]
Genome
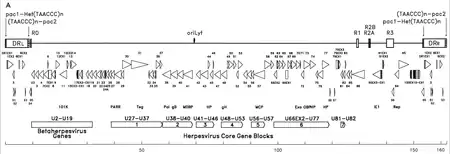
The genetic material of HHV-6 is composed of linear (circular during an active infection), double stranded DNA which contains an origin of replication, two 8–10 kb left and right direct repeat termini, and a unique segment that is 143–145kb.[22]
The origin of replication (often labeled as "oriLyt" in the literature) is where DNA replication begins.[21] The direct repeat termini (DRL and DRR) possess a repeated TTAGGG sequence, identical to that of human telomeres. Variability in the number of telomeric repeats is observed in the range of 15–180.[23][24] These termini also contain pac-1 and pac-2 cleavage and packing signals that are conserved among herpesviruses.
The unique segment contains seven major core gene blocks (U27-U37, U38-U40, U41-U46, U48-U53, U56-U57, U66EX2-U77, and U81-U82),[21] which is also characteristic of herpesviruses. These conserved genes code for proteins that are involved in replication, cleavage, and packing of the viral genome into a mature virion.[23] Additionally, they code for a number of immunomodulatory proteins. The unique segment also possesses a block of genes (U2-U19) that are conserved among HHV-6, HHV-7, and Cytomegaloviruses (the betaherpesviruses). A number of the unique segment genes are associated with, for instance, the HCMV US22 family (InterPro: IPR003360). The table below outlines some of their known properties.[21]
Genes
| Gene | Stage | Properties |
|---|---|---|
| IE-A (IE1? U89?) | Immediate early | Part of IE locus [25] — impairs interferon gene expression to restrict the development of cellular anti-viral measures, favoring a successful infection — not in membrane — activates viral DNA polymerases, involved in rolling circle replication — expression of this gene may be modulated by micro RNAs [26] |
| IE-B | Immediate early | Part of IE locus [25] Activates viral DNA polymerases, involved in rolling circle replication |
| DR1 | HCMV US22 gene family | |
| DR6 | HCMV US22 gene family, transactivator, oncogene | |
| DR7/U1 | SR domain, malignant transforming activity, binds to p53 | |
| U2 | HCMV US22 gene family — tegument protein | |
| U3 | HCMV UL24 homolog, HCMV US22 gene family, tegument protein — transactivating activity [25] | |
| U4 | HCMV Maribavir resistance | |
| U7 | HCMV US22 gene family | |
| U10 | dUTPase family | |
| U11 | Strongly immunoreactive virion protein [21] — antigenic tegument protein | |
| U12 | Chemokine G protein-coupled receptor | |
| U13 | CMV: Represses US3 transcription | |
| U14 | Binds and incorporates p53 into viral particles — HCMV UL25 gene family — antigenic tegument protein | |
| U15 | HCMV UL25 gene family | |
| U17 | HCMV UL25 gene family — tegument protein | |
| U18 | IE-B | Membrane glycoprotein |
| U19 | IE-B protein | Glycoprotein |
| U20 | Glycoprotein (specific to Roseolovirus) predicted immunoglobulin structure | |
| U21 | Binds to MHC-1 molecules and prevents antigen presenting cells from presenting HHV-6 peptides — glycoprotein, downregulates HLA I (specific to Roseolovirus) | |
| U22 | Late gene | Glycoprotein (absent from HHV-7, specific to Roseolovirus) |
| U23 | Glycoprotein (specific to Roseolovirus) | |
| U24 | Inhibits proper T cell activation, reducing secretion of cytokines at infection site — phosphorylation target for kinases — glycoprotein M (gM) (specific to Roseolovirus) | |
| U25 | HCMV UL22 gene family, tegument protein | |
| U26 | Putative multiple transmembrane protein | |
| U27 | DNA polymerase processivity factory | |
| U28 | Ribonucleotide reductase large subunit, tegument protein | |
| U29 | Capsid assembly and DNA maturation | |
| U30 | Tegument protein | |
| U31 | Large tegument protein | |
| U32 | Capsid protein, hexon tips | |
| U33 | Virion protein | |
| U34 | Membrane-associated phosphoprotein, primary envelopment | |
| U35 | Terminase component, DNA packaging | |
| U36 | DNA packaging | |
| U37 | Tegument protein, primary envelopment, phosphoprotein | |
| U38 | DNA polymerase | |
| U39 (gB, gp116) | Glycoprotein | |
| U40 | Transport, capsid assembly | |
| U41 | Early gene | Major DNA binding protein |
| U42 | Tegument protein, cell cycle block, transactivator | |
| U43 | DNA Helicase-primase complex | |
| U44 | Tegument protein | |
| U45 | dUTPase | |
| U46 | Glycoprotein N, membrane protein | |
| U47 (gO, O) | Glycoprotein O, associates with lipid rafts, exists in two forms, gO-120K and gO-80K, and gO-80K contains complex type N-linked oligosaccharides which are incorporated into viral particles | |
| U48 (gH, gp100) | Glycoprotein gH, virion constituent, part of CD46 gQ1/gQ2/gL/gH ligand complex, associates with lipid rafts | |
| U49 | Virion-associated regulatory protein, fusion protein | |
| U50 | DNA packaging | |
| U51 | Early gene | G protein-coupled chemokine receptor, preventing expression greatly reduces replication — increases intracellular levels of second messenger inositol phosphate, promotes chemotaxis – early gene, along with U41 and U69 [7] |
| U52 | ||
| U53 | Protease,[25] capsid assembly protein | |
| U54 | Tegument protein, virion transactivator | |
| U55 | Role in RNA synthesis, dUTPase | |
| U56 | Capsid protein | |
| U57 | Major capsid protein | |
| U58 | ||
| U59 | Tegument protein | |
| U61 | ||
| U62 | ||
| U63 | ||
| U64 | DNA packaging: tegument protein | |
| U65 | Tegument protein | |
| U66 | Terminase component | |
| U69 | Early gene | Tegument protein kinase (Ganciclovir kinase) involved in replication [25] |
| U70 | Alkaline exonuclease | |
| U71 | Myristylated virion protein | |
| U72 (gM) | Glycoprotein M | |
| U73 | Origin-binding protein | |
| U74 | DNa helicase-primase complex | |
| U75 | Tegument protein | |
| U76 | DNA packaging, virion protein | |
| U77 | Helicase-primase complex | |
| U79 | Transcriptional activation | |
| U80 | Predicted immunoglobulin structure | |
| U81 | Uracil-DNA glycosylase | |
| U82 (gL, gp80) | Glycoprotein L, virion constituent, part of CD46 gQ1/gQ2/gL/gH ligand complex, associates with lipid rafts | |
| U83 | Secreted chemotactic (chemoattractant) glycoprotein, binds to chemokine receptors, recruits host cells that secrete chemokines specific to U51 | |
| U85 | Glycoprotein (specific to Roseolovirus) | |
| U86 | IE-2 | IE-2 transactivator |
| U88 | IE-A | |
| U90 | IE-A (IE 1) | Transactivator |
| U91 | IE-A, Glycoprotein | |
| U94 | Latency (immediate early or early gene) | Involved in transcriptional repression of lytic genes – aids in the specific integration of HHV-6A/HHV-6B into the telomeres — highly expressed during latency — parvovirus rep homolog (absent in HHV-7) |
| U95 | CMV US22 gene family – colocalizes and interacts with the mitochondrial GRIM-19 protein, an essential component of the oxidative phosphorylation system [7] — binds to nuclear factor-kappa B (NF-κB), deregulation of which has been postulated to contribute to cancer [14] | |
| U100 (Gp82-105) | Late gene | Glycoprotein Q, virion constituent, associates with lipid rafts |
| gQ1 | Glycoprotein, complexes with gH and gL to form viral ligand to CD46 receptor – modified by N-glycosylation — expressed in two different forms: an 80-kDa form (gQ1-80K) and a 74-kDa form (gQ1-74K) – only gQ1-80K, but not gQ1-74K, forms the CD46 ligand complex with gQ2, gH, and gL [27] Associates with lipid rafts. | |
| gM1 | Lipid-raft-specific ganglioside, incorporated into virion | |
| gQ2 | Glycoprotein, forms gH/gL/gQ1/gQ2 complex, part of receptor ligand – essential for viral growth, associates with lipid rafts — exists in two forms: gQ2-34K and gQ2-37K | |
| Micro RNAs | hhv6b-miR-Ro6-1, -Ro6-2, -Ro6-3, and -Ro6-4. May regulate early transcription | |
| P100 aka p101 | Immunogenic, constituent of tegument | |
| ORF-1 (DR7) | Binds and inhibits transcriptional activity of p53 – can transform human epidermal keratinocytes and NIH 3T3 cells in vitro – cells expressing ORF-1 protein produce fibrosarcomas when injected into nude mice |
Viral entry
HHV-6 receptor
When an extracellular HHV-6 virion comes across human cells, it encounters the human receptor protein cluster of differentiation 46 (CD46), which plays a role in regulating the complement system. The CD46 protein possesses a single variable region, as a result of alternative splicing. As such, at least fourteen isoforms of CD46 exist, all of which bind HHV-6a.[28]
The extracellular region of CD46 contains four short consensus repeats of about 60 amino acids that fold into a compact beta-barrel domain surrounded by flexible loops.[23] As has been demonstrated for CD46 with other ligands, the CD46 protein structure linearizes upon binding HHV-6. While their precise interaction has not yet been determined, the second and third SCR domains have been demonstrated as required for HHV-6 receptor binding and cellular entry.
HHV-6 receptor ligand
Mori et al. first identified the gene product gQ1, a glycoprotein unique to HHV-6, and found that it forms a complex with gH and gL glycoproteins.[12][29] They believed that this heterotrimer complex served as the viral ligand for CD46.[22] Soon thereafter, another glycoprotein named gQ2 was identified and found to be part of the gH/gL/gQ1 ligand complex, forming a heterotetramer that was positively identified as the viral CD46 ligand.[29] The exact process of entry is not yet well understood.
Salivary glands
The salivary glands have been described as an in vivo reservoir for HHV-6 infection.[23]
Leukocytes
Researchers[30] have shown that T cells are highly infectable by HHV-6.
Nervous system
During the year 2011, researchers at the National Institutes of Health attempted to elucidate the then unknown method whereby HHV-6a gains entry into the nervous system. As such, they autopsied the brains of around 150 subjects. When various anatomical regions were assayed for their viral load, olfactory tissues were found to have the highest HHV-6 content. They concluded that these tissues are the entry point for HHV-6a.[16]
The results above are consistent with those of previous studies that involved HSV-1 (and a number of other viruses), which also disseminates into the CNS through olfactory tissue.[31]
Researchers also hypothesized that olfactory ensheathing cells (OECs), a group of specialized glial cells found in the nasal cavity, may have a role in HHV-6 infectivity.[16] They suspected this association as a result of OECs having properties similar to those of astrocytes, another type of glial cell that was previously identified as being susceptible to HHV-6 infection.[32] Research continued by infecting OECs in vitro with both types of HHV-6. Ultimately, only OECs in which HHV-6a was used tested positive for signs of de novo viral synthesis, as is also characteristic of astrocytes.[32]
Cellular activity
Once inside, two outcomes have been described: active and inactive infections.
Active infection
Active infections involve the linear dsDNA genome circularizing by end to end covalent linkages. This process was first reported for the herpes simplex virus.[24] Once circularized, HHV-6 begins to express what are known as "immediate early" genes. These gene products are believed to be transcription activators[7] and may be regulated by the expression of viral micro RNAs.[26] Subsequent expression of "early genes" then occurs and activates, for instance, viral DNA polymerases. Early genes are also involved in the rolling circle replication that follows.[23]
HHV-6's replication results in the formation of concatemers, which are long molecules that contain several repeats of a DNA sequence.[33] These long concatemers are then cleaved between the pac-1 and pac-2 regions by ribozymes for packaging of the genome into individual virions.[24]
Inactive infection
Not all newly infected cells begin rolling circle replication. In fact, herpes comes from the Greek word herpein, meaning "to creep." Herpesviruses are 'to creep' in that they may enter a latent stage, inactively infecting their human host. Since its discovery in 1993, this phenomenon has been found among all of the betaherpesviruses.[34]
Other betaherpesviruses establish latency as a nuclear episome, which is a circular DNA molecule (analogous to plasmids). For HHV-6, latency is believed to occur exclusively through the integration of viral telomeric repeats into human subtelomeric regions.[15] Only one other virus, Marek's disease virus, is known to achieve latency in this fashion.[7] This phenomenon is possible as a result of the telomeric repeats found within the direct repeat termini of HHV-6's genome.
The right direct repeat terminus integrates within 5 to 41 human telomere repeats, and preferentially does so into the proximal end[35] of chromosomes 9, 17, 18, 19, and 22, but has also occasionally been found in chromosomes 10 and 11.[33] Nearly 70 million individuals are suspected to carry chromosomally integrated HHV-6.[15][33]
A number of genes expressed by HHV-6 are unique to its inactive latency stage. These genes involve maintaining the genome and avoiding destruction of the host cell.[35] For instance, the U94 protein is believed to repress genes that are involved in cellular lysis (apoptosis) and also may aid in telomeric integration.[23] Once stored in human telomeres, the virus is reactivated intermittently.[35]
Reactivation
The specific triggers for reactivation are not well understood. Some researchers have suggested that injury, physical or emotional stress, and hormonal imbalances could be involved.[36]
Researchers during 2011 discovered that reactivation can positively be triggered in vitro by histone deacetylase inhibitors. Once reactivation begins, the rolling circle process is initiated and concatemers are formed as described above.[23]
Interactions
Human herpesvirus 6 lives primarily on humans and, while variants of the virus can cause mild to fatal illnesses, can live commensally on its host.[13] It has been demonstrated that HHV-6 fosters the progression of HIV-1 upon coinfection in T cells.[37] HHV-6 upregulates the expression of the primary HIV receptor CD4, thus expanding the range of HIV susceptible cells. Several studies also have shown that HHV-6 infection increases production of inflammatory cytokines that enhance in vitro expression of HIV-1, such as TNF-alpha,[38] IL-1 beta, and IL-8.[39] A more recent in vivo study shows HHV-6A coinfection to dramatically accelerate the progression from HIV to AIDS in pigtailed macaques.[40]
HHV-6 has also been demonstrated to transactivate Epstein–Barr virus.[31]
Epidemiology
Age
Humans acquire the virus at an early age, some as early as less than one month of age. HHV-6 primary infections account for up to 20% of infant emergency room visits for fever in the United States[41][42] and are associated with several more severe complications, such as encephalitis, lymphadenopathy, myocarditis and myelosuppression. The prevalence of the virus in the body increases with age (rates of infection are highest among infant between 6 and 12 months old) and it is hypothesized that this is due to the loss of maternal antibodies in a child that protect him or her from infections.[13]
There are inconsistencies with the correlations between age and seropositivity: According to some reports there is a decrease of seropositivity with the increase of age, while some indicate no significant decline, and others report an increased rate of seropositivity for individuals age 62 and older. After primary infection, latency is established in salivary glands, hematopoietic stem cells, and other cells, and exists for the lifetime of the host.
Geographical distribution
The virus is known to be widespread around the world. An HHV-6 infection rate of 64-83% by age 13 months has been reported for countries including the United States, United Kingdom, Japan and Taiwan.[13][43] Studies have found seroprevalence varying "from approximately 39 to 80% among ethnically diverse adult populations from Tanzania, Malaysia, Thailand, and Brazil."[13] There are no significant differences among ethnic groups living in the same geographical location or between sexes. While HHV-6B is present in almost all of the world's populations, HHV-6A appears to be less frequent in Japan, North America, and Europe.[13]
Transmission
Transmission is believed to occur most frequently through the shedding of viral particles into saliva. Both HHV-6B and HHV-7 are found in human saliva, the former being at a lower frequency. Studies report varying rates of prevalence of HHV-6 in saliva (between 3–90%),[13] and have also described the salivary glands as an in vivo reservoir for HHV-6. The virus infects the salivary glands, establishes latency, and periodically reactivates to spread infection to other hosts.[23]
Vertical transmission has also been described, and occurs in approximately 1% of births in the United States.[7][44] This form is easily identifiable as the viral genome is contained within every cell of an infected individual.
Diagnosis
The diagnosis of HHV-6 infection is performed by both serologic and direct methods. The most prominent technique is the quantification of viral DNA in blood, other body fluids, and organs by means of real-time PCR.[45]
Clinical significance
The classical presentation of primary HHV-6b infection is as exanthema subitum (ES) or "roseola", featuring a high temperature followed by a rash. However, one study (1997) indicated that a rash is not a distinguishing feature of HHV-6 infection, with rates similar to non-HHV-6 infections (10–20% of febrile children in both groups). HHV-6 infections more frequently present with high temperatures (over 40C), at a rate of around two thirds compared to less than half in the non-HHV-6 patients. Similarly significant differences were seen in malaise, irritability, and tympanic membrane inflammation.[13]
Primary infection in adults tend to be more severe.[13]
Diagnosis for the virus, particularly HHV-6B, is vital for the patient because of the infection's adverse effects. Symptoms that point to this infection, such as rashes, go unnoticed in patients that receive antibiotics because they can be misinterpreted as a side-effect of the medicine.[13] HHV-6B is known to be associated with the childhood disease roseola infantum, as well as other illnesses caused by the infection. These include hepatitis, febrile convulsions, and encephalitis. Children who suffer from exanthema subitum, caused by an HHV-6B infection, experience fevers lasting 3 to 5 days; rashes on the torso, neck, and face; and sometimes febrile convulsions, however, the symptoms are not always present together. Primary infections in adults are rare since most occurrences are in children. When the infection does occur for the first time in an adult the symptoms can be severe.
The virus periodically re-activates from its latent state, with HHV-6 DNA being detectable in 20–25% of healthy adults in the United States. In the immunocompetent setting, these re-activations are often asymptomatic, but in immunosuppressed individuals there can be serious complications. HHV-6 re-activation causes severe disease in transplant recipients and can lead to graft rejection, often in consort with other betaherpesviridae. Likewise in HIV/AIDS, HHV-6 re-activations cause disseminated infections leading to end organ disease and death. Although up to 100% of the population are exposed (seropositive) to HHV-6, most by 3 years of age, there are rare cases of primary infections in adults. In the United States, these have been linked more with HHV-6a, which is thought to be more pathogenic and more neurotropic and has been linked to several central nervous system-related disorders.
HHV-6 has been reported in multiple sclerosis patients[46] and has been implicated as a co-factor in several other diseases, including chronic fatigue syndrome,[47] fibromyalgia, AIDS,[48] optic neuritis, cancer, and temporal lobe epilepsy.[49]
Multiple sclerosis
Multiple sclerosis (MS) is an autoimmune and inflammatory disorder of the nervous system that results in demyelination of axons in the brain and spinal cord. The history of MS in the context of HHV-6 began during 1995 when Peter Challoner, a scientist at PathoGenesis Corporation of Seattle, began looking for non-human genetic sequences in the brains of MS patients. He found an unusually high expression of HHV-6 DNA within oligodendrocytes. He also noticed a higher concentration of infected cells in areas where demyelination had occurred.[50] His research was likely the first published study to suggest a link between HHV-6 and MS.
Epidemiological data
MS prevalence increases in populations as they are farther from the Equator.[51][52] Incidence is three times higher in those born 42 degrees latitude north and above than in those born 37 degrees north and below. Individuals are also less likely to present with MS as an adult if their childhood was spent in a low incidence region. The possibility of a causative infectious agent in association with MS has been evaluated through the lens of these epidemiological findings.
To explain the data above, two hypotheses were proposed.[53] The first is known as the Poliomyelitis hypothesis and suggests that infection at a young age confers immunity but adult infection increases MS risk. The second is known as the Prevalence hypothesis, and suggests that MS is caused by a pathogen that is more common in regions with high rates of MS. This pathogen would be widespread and cause an asymptomatic (latent) infection in most individuals. Only rarely and years after the primary infection does this hypothetical agent cause the neurological symptoms of MS. A third hypothesis essentially combines these two and also suggests the involvement of multiple pathogens. The third may best apply to the epidemiological data.[53][54]
Possible viral involvement
The Epstein–Barr virus (EBV) paradox is also noteworthy, as HHV-6 has been reported to transactivate EBV.[31] Individuals are at a 10-fold less risk of MS if they are seronegative for EBV. However, among individuals who are positive, those that acquire EBV infection later in life are at a 3-fold greater risk for MS.
Research suggests that viral infections can be tied even closer to MS. EBV antibodies in healthy individuals remain constant, whereas antibody levels in individuals who later develop MS begin to increase and plateau between 20 and 30 years of age, regardless of age of onset.
More specific to HHV-6, researchers in 2004 discovered that the initial stages of MS are associated with high levels of the active virus.[55] Soon thereafter, researchers discovered that levels of active HHV-6 are also elevated during relapses/exacerbations of MS.[4]
Researchers have demonstrated that levels of HHV-6 IgG1 and IgM antibodies are elevated in MS patients relative to controls.[23] In fact, research published in 2014 found that increases in anti-HHV-6A/B IgG and IgM titers are predictive of MS relapse.[56]
Analysis of the epidemiological, serological, and immunological data above supports the association between an infectious agent and MS. However, the exact mechanism of a possible viral influence on the manifestation of MS is less clear. Although, a few mechanisms have been suggested: molecular mimicry, phosphorylation pathways, and cytokines.[16][57][58][59][60]
Molecular mimicry
The first study to specifically investigate HHV-6-related demyelination appeared in the literature during 1996, when a previously healthy 19-month-old child developed acute encephalopathy. Levels of myelin basic protein were elevated in his cerebrospinal fluid, suggesting that demyelination was occurring.[57] This link was almost forgotten, until four years later when an MS-related study was published showing an HHV-6 prevalence of 90% among demyelinated brain tissues. In comparison, a mere 13% of disease-free brain tissues possessed the virus.[61]
The molecular mimicry hypothesis, in which T cells are essentially confusing an HHV-6 viral protein with myelin basic protein, first appeared around this time. Early on in the development of this hypothesis (2002), Italian researchers used the HHV-6a variant along with bovine myelin basic protein to generate cross-reactive T cell lines. These were compared to the T cells of individuals with MS as well as those of controls, and no significant difference was found between the two. Their early research suggested that molecular mimicry may not be a mechanism that is involved in MS.[58]
A few months later, researchers in the United States created a synthetic peptide with a sequence identical to that of an HHV-6 peptide. They were able to show that T cells were activated by this peptide. These activated T cells also recognized and initiated an immune response against a synthetically created peptide sequence that is identical to part of human myelin basic protein. During their research, they found that the levels of these cross-reactive T cells are significantly elevated in MS patients.[59] Their research concluded by suggesting that HHV-6 may indeed be a causative agent for MS.
Several similar studies followed. A study from October 2014 supported the role of long-term HHV-6 infection with demyelination in progressive neurological diseases.[62]
Phosphorylation pathways
Myelin basic protein (MBP) regularly exchanges phosphate groups with the environment, and its ability to do so has implications for proper myelin sheath integrity. More specifically, two threonine residues on MBP have been identified as the phosphorylation targets of glycogen synthase kinase and mitogen-activated protein kinase. Their action on MBP is said to aid in its ability to polymerize and bundle myelin. Phosphorylated MBP is also more resistant to several proteases.[60]
Among individuals with MS, these target threonines have been found to be phosphorylated less often. In fact, HHV-6 produces a transmembrane protein, known as U24, that is also a phosphorylation target of the kinases mentioned previously. Our kinases act on an HHV-6 protein due to a shared sequence of seven amino acids (MBP92–104=IVTPRTPPPSQGK; U241–13=MDPPRTPPPSYSE). As a result, essential post-translational modifications may not be occurring for MBPs in individuals with active HHV-6 infections.[60]
- Multiple sclerosis – direct cell damage and altered cytokines
HHV-6 has been shown to infect olfactory ensheathing cells (OECs). OECs have been investigated thoroughly in relation to spinal cord injuries, amyotrophic lateral sclerosis, and other neurodegenerative diseases. Researchers suggest that these cells possess a unique ability to remyelinate injured neurons.[16]
Some of the genes expressed by HHV-6 manipulate host levels of various cytokines (see section on gene products). For instance, infected cells have increased levels of interleukin-8, which is believed to induce MMP-9 repression. Elevated levels of MMP-9 have been found among individuals with MS.[63]
HHV-6 reactivation has also been implicated in the exacerbation of MS via a shift in Th lymphocyte subsets.[64]
Chronic fatigue syndrome
Chronic fatigue syndrome (CFS) is a debilitating illness,[65] cause of which is unknown. Patients with CFS have abnormal neurological, immunological, and metabolic findings.
For many, but not all, patients who meet criteria for CFS, the illness begins with an acute, infectious-like syndrome. Cases of CFS can follow well-documented infections with several infectious agents.[66] A study of 259 patients with a "CFS-like" illness published shortly after HHV-6 was discovered used primary lymphocyte cultures to identify people with active replication of HHV-6. Such active replication was found in 70% of the patients vs. 20% of the control subjects ().[67] The question raised but not answered by this study was whether the illness caused subtle immune deficiency that led to reactivation of HHV-6, or whether reactivation of HHV-6 led to the symptoms of the illness.
Subsequent studies employing only serological techniques that do not distinguish active from latent infection have produced mixed results: most, but not all, have found an association between CFS and HHV-6 infection.[66][68][69]
Other studies have employed assays that can detect active infection: primary cell culture, PCR of serum or plasma, or IgM early antigen antibody assays. The majority of these studies have shown an association between CFS and active HHV-6 infection,[68][70][71][72][73][74] although a few have not.[69][75]
In summary, active infection with HHV-6 is present in a substantial fraction of patients with CFS. Moreover, HHV-6 is known to infect cells of the nervous system and immune system, organ systems with demonstrable abnormalities in CFS. Despite this association, it remains unproven that reactivated HHV-6 infection is a cause of CFS.
Hashimoto's thyroiditis
Hashimoto's thyroiditis is the most common thyroid disease and is characterized by abundant lymphocyte infiltrate and thyroid impairment. Recent research suggests a potential role for HHV-6 (possibly variant A) in the development or triggering of Hashimoto's thyroiditis.[76]
Pregnancy
The role of HHV-6 during pregnancy leading to inflammation in the amniotic cavity has been studied.[77]
Infertility
HHV-6A DNA was found in the endometrium of almost half of a group of infertile women, but in none of the fertile control group. Natural killer cells specific for HHV-6A, and high uterine levels of certain cytokines, were also found in the endometrium of the infertile women positive for HHV-6A. The authors suggest that HHV-6A may prove to be an important factor in female infertility.[78]
Cancer
Many human oncogenic viruses have been identified. For instance, HHV-8 is linked to Kaposi's sarcoma,[79] the Epstein–Barr virus to Burkitt's lymphoma, and HPV to cervical cancer. In fact, the World Health Organization estimated (2002) that 17.8% of human cancers were caused by infection.[80] The typical methods whereby viruses initiate oncogenesis involve suppressing the host's immune system, causing inflammation, or altering genes.
HHV-6 has been detected in lymphomas, leukemias, cervical cancers, and brain tumors.[14] Various medulloblastoma cell lines as well as the cells of other brain tumors have been demonstrated to express the CD46 receptor. Viral DNA has also been identified in many other non-pathological brain tissues, but the levels are lower.[14]
The human P53 protein functions as a tumor suppressor. Individuals who do not properly produce this protein experience a higher incidence of cancer, a phenomenon known as Li-Fraumeni syndrome. One of HHV-6's gene products, the U14 protein, binds P53 and incorporates it into virions. Another gene product, the ORF-1 protein, can also bind and inactivate P53. Cells expressing the ORF-1 gene have even been shown to produce fibrosarcomas when injected into mice.[14]
Another product of HHV-6, the immediate early protein U95, has been shown to bind nuclear factor-kappa B. Deregulation of this factor is associated with cancer.[14]
Optic neuritis
HHV-6 induced ocular inflammation has been reported three times. All three were reported in elderly individuals, two during 2007 and one during 2011. The first two were reported in Japan and France, the most recent one in Japan.[81][82][83]
These were believed to have occurred as a result of a reactivation, as anti-HHV-6 IgM antibody levels were low.[83]
Temporal lobe epilepsy
Epilepsy of the mesial temporal lobe is associated with HHV-6 infection. Within this region of the brain exists three structures: the amygdala, hippocampus, and parahippocampal gyrus. Mesial temporal lobe epilepsy (MTLE) is the most common form of chronic epilepsy and its underlying mechanism is not fully understood.[84]
Researchers consistently report having found HHV-6 DNA in tissues that were removed from patients with MTLE. Studies have demonstrated a tendency for HHV-6 to aggregate in the temporal lobe,[85] with the highest concentrations in astrocytes of the hippocampus.[84]
However, one group of researchers ultimately concluded that HHV-6 may not be involved in MTLE related to Mesial Temporal Sclerosis.[86]
Liver failure
The virus is a common cause of liver dysfunction and acute liver failure, and has recently been linked to periportal confluent necrosis. Furthermore, HHV-6 DNA is often detectable only in the biopsy tissues as DNA levels fall below the level of detection in blood in persistent cases.[87]
Treatment
There are no pharmaceuticals approved specifically for treating HHV-6 infection, although the usage of Cytomegalovirus treatments (valganciclovir, ganciclovir,[88] cidofovir, and foscarnet) have shown some success.[7] These drugs are given with the intent of inhibiting proper DNA polymerization by competing with deoxy triphosphate nucleotides[88] or specifically inactivating viral DNA polymerases.[2]
Finding a treatment can be difficult when HHV-6 reactivation occurs following transplant surgery because transplant medications include immunosuppressants.[89]
References
- Adams, M. J.; Carstens, E. B. (2012). "Ratification vote on taxonomic proposals to the International Committee on Taxonomy of Viruses (2012)". Archives of Virology. 157 (7): 1411–1422. doi:10.1007/s00705-012-1299-6. PMID 22481600.
- Jaworska, J.; Gravel, A.; Flamand, L. (2010). "Divergent susceptibilities of human herpesvirus 6 variants to type I interferons". Proceedings of the National Academy of Sciences. 107 (18): 8369–74. Bibcode:2010PNAS..107.8369J. doi:10.1073/pnas.0909951107. PMC 2889514. PMID 20404187.
- De Bolle, L.; Van Loon, J.; De Clercq, E.; Naesens, L. (2005). "Quantitative analysis of human herpesvirus 6 cell tropism". Journal of Medical Virology. 75 (1): 76–85. doi:10.1002/jmv.20240. PMID 15543581.
- Álvarez-Lafuente, Roberto; García-Montojo, Marta; De Las Heras, Virginia; Bartolomé, Manuel; Arroyo, Rafael (2006). "Clinical parameters and HHV-6 active replication in relapsing—remitting multiple sclerosis patients". Journal of Clinical Virology. 37: S24–6. doi:10.1016/S1386-6532(06)70007-5. PMID 17276363.
- Readhead, Ben; Haure-Mirande, Jean-Vianney; Funk, Cory C.; Richards, Matthew A.; Shannon, Paul; Haroutunian, Vahram; Sano, Mary; Liang, Winnie S.; Beckmann, Noam D.; Price, Nathan D.; Reiman, Eric M.; Schadt, Eric E.; Ehrlich, Michelle E.; Gandy, Sam; Dudley, Joel T. (June 2018). "Multiscale Analysis of Independent Alzheimer's Cohorts Finds Disruption of Molecular, Genetic, and Clinical Networks by Human Herpesvirus". Neuron. 99 (1): 64–82.e7. doi:10.1016/j.neuron.2018.05.023. PMC 6551233. PMID 29937276.
- Yoshikawa, Tetsushi (2004). "Human herpesvirus 6 infection in hematopoietic stem cell transplant patients". British Journal of Haematology. 124 (4): 421–32. doi:10.1046/j.1365-2141.2003.04788.x. PMID 14984492.
- Flamand, Louis; Komaroff, Anthony L.; Arbuckle, Jesse H.; Medveczky, Peter G.; Ablashi, Dharam V. (2010). "Review, part 1: Human herpesvirus-6-basic biology, diagnostic testing, and antiviral efficacy". Journal of Medical Virology. 82 (9): 1560–8. doi:10.1002/jmv.21839. PMID 20648610.
- Anderson, L. (1988). "Human Retrovirus Family: Cancer, Central Nervous System Disease, and AIDS". JNCI Journal of the National Cancer Institute. 80 (13): 987–9. doi:10.1093/jnci/80.13.987. PMID 2842514.
- Salahuddin, S.; Ablashi, D.; Markham, P.; Josephs, S.; Sturzenegger, S; Kaplan, M; Halligan, G; Biberfeld, P; et al. (1986). "Isolation of a new virus, HBLV, in patients with lymphoproliferative disorders". Science. 234 (4776): 596–601. Bibcode:1986Sci...234..596Z. doi:10.1126/science.2876520. PMID 2876520.
- Ablashi, DV; Salahuddin, SZ; Josephs, SF; Imam, F; Lusso, P; Gallo, RC; Hung, C; Lemp, J; Markham, PD (1987). "HBLV (or HHV-6) in human cell lines". Nature. 329 (6136): 207. Bibcode:1987Natur.329..207A. doi:10.1038/329207a0. PMID 3627265.
- Ablashi, Dharam; Krueger, Gerhard (2006). Human Herpesvirus-6 General Virology, Epidemiology and Clinical Pathology (2nd ed.). Burlington: Elsevier. p. 7. ISBN 9780080461281.
- Kawabata, A.; Oyaizu, H.; Maeki, T.; Tang, H.; Yamanishi, K.; Mori, Y. (2011). "Analysis of a Neutralizing Antibody for Human Herpesvirus 6B Reveals a Role for Glycoprotein Q1 in Viral Entry". Journal of Virology. 85 (24): 12962–71. doi:10.1128/JVI.05622-11. PMC 3233151. PMID 21957287.
- Braun, DK; Dominguez, G; Pellett, PE (1997). "Human herpesvirus 6". Clinical Microbiology Reviews. 10 (3): 521–67. doi:10.1128/CMR.10.3.521. PMC 172933. PMID 9227865.
- Kofman, Alexander; Marcinkiewicz, Lucasz; Dupart, Evan; Lyshchev, Anton; Martynov, Boris; Ryndin, Anatolii; Kotelevskaya, Elena; Brown, Jay; et al. (2011). "The roles of viruses in brain tumor initiation and oncomodulation". Journal of Neuro-Oncology. 105 (3): 451–66. doi:10.1007/s11060-011-0658-6. PMC 3278219. PMID 21720806.
- Arbuckle, J. H.; Medveczky, M. M.; Luka, J.; Hadley, S. H.; Luegmayr, A.; Ablashi, D.; Lund, T. C.; Tolar, J.; et al. (2010). "The latent human herpesvirus-6A genome specifically integrates in telomeres of human chromosomes in vivo and in vitro". Proceedings of the National Academy of Sciences. 107 (12): 5563–5568. Bibcode:2010PNAS..107.5563A. doi:10.1073/pnas.0913586107. PMC 2851814. PMID 20212114.
- Harberts, E.; Yao, K.; Wohler, J. E.; Maric, D.; Ohayon, J.; Henkin, R.; Jacobson, S. (2011). "Human herpesvirus-6 entry into the central nervous system through the olfactory pathway". Proceedings of the National Academy of Sciences. 108 (33): 13734–9. Bibcode:2011PNAS..10813734H. doi:10.1073/pnas.1105143108. PMC 3158203. PMID 21825120.
- Fenner, F. (1971). "The nomenclature and classification of viruses the International Committee on Nomenclature of Viruses". Virology. 46 (3): 979–980. doi:10.1016/0042-6822(71)90102-4. PMID 18619371.
- Fenner, F. (1976). "Classification and nomenclature of viruses. Second report of the International Committee on Taxonomy of Viruses". Intervirology. 7 (1–2): 1–115. doi:10.1159/000149938. PMID 826499.
- Davison AJ (2010) Herpesvirus systematics. Vet. Microbiol. 143(1–2): 52–69
- Kawabata, Akiko; Tang, Huamin; Huang, Honglan; Yamanishi, Koichi; Mori, Yasuko (2009). "Y Human herpesvirus 6 envelope components enriched in lipid rafts: Evidence for virion-associated lipid rafts". Virology Journal. 6: 127. doi:10.1186/1743-422X-6-127. PMC 2743664. PMID 19689819.
- Dominguez, G.; Dambaugh, T. R.; Stamey, F. R.; Dewhurst, S.; Inoue, N.; Pellett, P. E. (1999). "Human herpesvirus 6B genome sequence: Coding content and comparison with human herpesvirus 6A". Journal of Virology. 73 (10): 8040–8052. doi:10.1128/JVI.73.10.8040-8052.1999. PMC 112820. PMID 10482553.
- Tang, Huamin; Kawabata, Akiko; Yoshida, Mayumi; Oyaizu, Hiroko; Maeki, Takahiro; Yamanishi, Koichi; Mori, Yasuko (2010). "Human herpesvirus 6 encoded glycoprotein Q1 gene is essential for virus growth". Virology. 407 (2): 360–7. doi:10.1016/j.virol.2010.08.018. PMID 20863544.
- Arbuckle, Jesse H.; Medveczky, Peter G. (2011). "The molecular biology of human herpesvirus-6 latency and telomere integration". Microbes and Infection. 13 (8–9): 731–41. doi:10.1016/j.micinf.2011.03.006. PMC 3130849. PMID 21458587.
- Borenstein, R.; Frenkel, N. (2009). "Cloning human herpes virus 6A genome into bacterial artificial chromosomes and study of DNA replication intermediates". Proceedings of the National Academy of Sciences. 106 (45): 19138–19143. Bibcode:2009PNAS..10619138B. doi:10.1073/pnas.0908504106. PMC 2767366. PMID 19858479.
- Yoshikawa, Tetsushi; Asano, Yoshizo; Akimoto, Shiho; Ozaki, Takao; Iwasaki, Takuya; Kurata, Takeshi; Goshima, Fumi; Nishiyama, Yukihiro (2002). "Latent infection of human herpesvirus 6 in astrocytoma cell line and alteration of cytokine synthesis". Journal of Medical Virology. 66 (4): 497–505. doi:10.1002/jmv.2172. PMID 11857528.
- Tuddenham, L.; Jung, J. S.; Chane-Woon-Ming, B.; Dolken, L.; Pfeffer, S. (2011). "Small RNA Deep Sequencing Identifies MicroRNAs and Other Small Noncoding RNAs from Human Herpesvirus 6B". Journal of Virology. 86 (3): 1638–49. doi:10.1128/JVI.05911-11. PMC 3264354. PMID 22114334.
- Tang, H.; Hayashi, M.; Maeki, T.; Yamanishi, K.; Mori, Y. (2011). "Human Herpesvirus 6 Glycoprotein Complex Formation is Required for Folding and Trafficking of the gH/gL/gQ1/gQ2 Complex and Its Cellular Receptor Binding". Journal of Virology. 85 (21): 11121–30. doi:10.1128/JVI.05251-11. PMC 3194968. PMID 21849437.
- Greenstone, H. L.; Santoro, F; Lusso, P; Berger, EA (2002). "Human Herpesvirus 6 and Measles Virus Employ Distinct CD46 Domains for Receptor Function". Journal of Biological Chemistry. 277 (42): 39112–8. doi:10.1074/jbc.M206488200. PMID 12171934.
- Mori, Yasuko (2009). "Recent topics related to human herpesvirus 6 cell tropism". Cellular Microbiology. 11 (7): 1001–6. doi:10.1111/j.1462-5822.2009.01312.x. PMID 19290911.
- J Exp Med. 1995 Apr 1;181(4):1303–10. Infection of gamma/delta T lymphocytes by human herpesvirus 6: transcriptional induction of CD4 and susceptibility to HIV infection. Lusso P, Garzino-Demo A, Crowley RW, Malnati MS.
- Liedtke, W.; Opalka, B.; Zimmermann, C.W.; Lignitz, E. (1993). "Age distribution of latent herpes simplex virus 1 and varicella-zoster virus genome in human nervous tissue". Journal of the Neurological Sciences. 116 (1): 6–11. doi:10.1016/0022-510X(93)90082-A. PMID 8389816.
- Cassiani-Ingoni, Riccardo; Greenstone, Heather L.; Donati, Donatella; Fogdell-Hahn, Anna; Martinelli, Elena; Refai, Daniel; Martin, Roland; Berger, Edward A.; Jacobson, Steven (2005). "CD46 on glial cells can function as a receptor for viral glycoprotein-mediated cell-cell fusion". Glia. 52 (3): 252–8. doi:10.1002/glia.20219. PMID 15920733.
- Morissette, G.; Flamand, L. (2010). "Herpesviruses and Chromosomal Integration". Journal of Virology. 84 (23): 12100–9. doi:10.1128/JVI.01169-10. PMC 2976420. PMID 20844040.
- Potenza, Leonardo; Barozzi, Patrizia; Torelli, Giuseppe; Luppi, Mario (2010). "Translational challenges of human herpesvirus 6 chromosomal integration". Future Microbiology. 5 (7): 993–5. doi:10.2217/fmb.10.74. hdl:11380/704738. PMID 20632798.
- Kaufer, B. B.; Jarosinski, K. W.; Osterrieder, N. (2011). "Herpesvirus telomeric repeats facilitate genomic integration into host telomeres and mobilization of viral DNA during reactivation". Journal of Experimental Medicine. 208 (3): 605–15. doi:10.1084/jem.20101402. PMC 3058580. PMID 21383055.
- Isegawa, Yuji; Matsumoto, Chisa; Nishinaka, Kazuko; Nakano, Kazushi; Tanaka, Tatsuya; Sugimoto, Nakaba; Ohshima, Atsushi (2010). "PCR with quenching probes enables the rapid detection and identification of ganciclovir-resistance-causing U69 gene mutations in human herpesvirus 6". Molecular and Cellular Probes. 24 (4): 167–77. doi:10.1016/j.mcp.2010.01.002. PMID 20083192.
- Lusso, Paolo; De Maria, Andrea; Malnati, Mauro; Lori, Franco; Derocco, Susan E.; Baseler, Michael; Gallo, Robert C. (1991). "Induction of CD4 and susceptibility to HIV-1 infection in human CD8+ T lymphocytes by human herpesvirus 6". Nature. 349 (6309): 533–5. Bibcode:1991Natur.349..533L. doi:10.1038/349533a0. PMID 1846951.
- Arena, A; Liberto, MC; Capozza, AB; Focà, A (1997). "Productive HHV-6 infection in differentiated U937 cells: Role of TNF alpha in regulation of HHV-6". The New Microbiologica. 20 (1): 13–20. PMID 9037664.
- Inagi, Reiko; Guntapong, Ratigorn; Nakao, Masayuki; Ishino, Yoshizumi; Kawanishi, Kazunobu; Isegawa, Yuji; Yamanishi, Koichi (1996). "Human herpesvirus 6 induces IL-8 gene expression in human hepatoma cell line, Hep G2". Journal of Medical Virology. 49 (1): 34–40. doi:10.1002/(SICI)1096-9071(199605)49:1<34::AID-JMV6>3.0.CO;2-L. PMID 8732869.
- Lusso, P.; Crowley, R. W.; Malnati, M. S.; Di Serio, C.; Ponzoni, M.; Biancotto, A.; Markham, P. D.; Gallo, R. C. (2007). "Human herpesvirus 6A accelerates AIDS progression in macaques". Proceedings of the National Academy of Sciences. 104 (12): 5067–72. Bibcode:2007PNAS..104.5067L. doi:10.1073/pnas.0700929104. JSTOR 25427145. PMC 1829265. PMID 17360322.
- Hall, Caroline Breese; Long, Christine E.; Schnabel, Kenneth C.; Caserta, Mary T.; McIntyre, Kim M.; Costanzo, Maria A.; Knott, Anne; Dewhurst, Stephen; et al. (1994). "Human Herpesvirus-6 Infection in Children -- A Prospective Study of Complications and Reactivation". New England Journal of Medicine. 331 (7): 432–8. doi:10.1056/NEJM199408183310703. PMID 8035839.
- Newly Found Herpes Virus Is Called Major Cause of Illness in Young, New York Times
- Okuno, T; Takahashi, K; Balachandra, K; Shiraki, K; Yamanishi, K; Takahashi, M; Baba, K (1989). "Seroepidemiology of human herpesvirus 6 infection in normal children and adults". Journal of Clinical Microbiology. 27 (4): 651–3. doi:10.1128/JCM.27.4.651-653.1989. PMC 267390. PMID 2542358.
- Araujo, A.; Pagnier, A.; Frange, P.; Wroblewski, I.; Stasia, M.-J.; Morand, P.; Plantaz, D. (2011). "Syndrome d'activation lymphohistiocytaire associé à une infection à Burkholderia cepacia complex chez un nourrisson révélant une granulomatose septique et une intégration génomique du virus HHV-6" [Lymphohistiocytic activation syndrome and Burkholderia cepacia complex infection in a child revealing chronic granulomatous disease and chromosomal integration of the HHV-6 genome]. Archives de Pédiatrie (in French). 18 (4): 416–9. doi:10.1016/j.arcped.2011.01.006. PMID 21397473.
- Agut Henri, Bonnafous Pascale, Gautheret-Dejean Agnès (2015). "Laboratory and Clinical Aspects of Human Herpesvirus 6 Infections". Clinical Microbiology Reviews. 28: 313–335. doi:10.1128/CMR.00122-14.CS1 maint: multiple names: authors list (link)
- Alvarez-Lafuente, R.; Martin-Estefania, C.; De Las Heras, V.; Castrillo, C.; Cour, I.; Picazo, J.J.; Varela De Seijas, E.; Arroyo, R. (2002). "Prevalence of herpesvirus DNA in MS patients and healthy blood donors". Acta Neurologica Scandinavica. 105 (2): 95–9. doi:10.1034/j.1600-0404.2002.1o050.x. PMID 11903118.
- Komaroff, Anthony L. (2006). "Is human herpesvirus-6 a trigger for chronic fatigue syndrome?". Journal of Clinical Virology. 37: S39–46. doi:10.1016/S1386-6532(06)70010-5. PMID 17276367.
- HHV-6 and AIDS Archived 8 February 2007 at the Wayback Machine, Wisconsin Viral Research Group
- Fotheringham, Julie; Donati, Donatella; Akhyani, Nahid; Fogdell-Hahn, Anna; Vortmeyer, Alexander; Heiss, John D.; Williams, Elizabeth; Weinstein, Steven; et al. (2007). "Association of Human Herpesvirus-6B with Mesial Temporal Lobe Epilepsy". PLOS Medicine. 4 (5): e180. doi:10.1371/journal.pmed.0040180. PMC 1880851. PMID 17535102.
- Challoner, Peter B.; Smith, Kirsten T.; Parker, Jay D.; MacLeod, David L.; Coulter, Silvija N.; Rose, Timothy M.; Schultz, Emily R.; Lindsley Bennett, J.; et al. (1995). "Plaque-Associated Expression of Human Herpesvirus 6 in Multiple Sclerosis". Proceedings of the National Academy of Sciences of the United States of America. 92 (16): 7440–4. Bibcode:1995PNAS...92.7440C. doi:10.1073/pnas.92.16.7440. PMC 41355. PMID 7638210.
- Compston, Alastair; Coles, Alasdair (2008). "Multiple sclerosis". The Lancet. 372 (9648): 1502–17. doi:10.1016/S0140-6736(08)61620-7. PMID 18970977.
- Compston, Alastair; Coles, Alasdair (2002). "Multiple sclerosis". The Lancet. 359 (9313): 1221–31. doi:10.1016/S0140-6736(02)08220-X. PMID 11955556.
- Hernán, Miguel A.; Zhang, Shumin M.; Lipworth, Loren; Olek, Michael J.; Ascherio, Alberto (2001). "Multiple Sclerosis and Age at Infection with Common Viruses". Epidemiology. 12 (3): 301–6. doi:10.1097/00001648-200105000-00009. PMID 11337603.
- Delbue, Serena; Carluccio, Silvia; Ferrante, Pasquale (2012). "The long and evolving relationship between viruses and multiple sclerosis". Future Virology. 7 (9): 871–83. doi:10.2217/fvl.12.78.
- Rotola, A; Merlotti, I; Caniatti, L; Caselli, E; Granieri, E; Tola, MR; Di Luca, D; Cassai, E (2004). "Human herpesvirus 6 infects the central nervous system of multiple sclerosis patients in the early stages of the disease". Multiple Sclerosis. 10 (4): 348–54. doi:10.1191/1352458504ms1045oa. PMID 15327028.
- Ortega-Madueno, I.; Garcia-Montojo, M.; Dominguez-Mozo, M.; Arias-Leal, A.; Casanova, I. (2014). "Anti-human herpesvirus 6A/B IgG correlates with relapses and progression in multiple sclerosis". PLOS One. 9 (8): e104836. Bibcode:2014PLoSO...9j4836O. doi:10.1371/journal.pone.0104836. PMC 4128748. PMID 25110949.
- Kamei, A.; Ichinohe, S.; Onuma, R.; Hiraga, S.; Fujiwara, T. (1997). "Acute disseminated demyelination due to primary human herpesvirus-6 infection". European Journal of Pediatrics. 156 (9): 709–12. doi:10.1007/s004310050695. PMID 9296535.
- Cirone, Mara; Cuomo, Laura; Zompetta, Claudia; Ruggieri, Stefano; Frati, Luigi; Faggioni, Alberto; Ragona, Giuseppe (2002). "Human herpesvirus 6 and multiple sclerosis: A study of t cell cross-reactivity to viral and myelin basic protein antigens". Journal of Medical Virology. 68 (2): 268–72. doi:10.1002/jmv.10190. PMC 7167112. PMID 12210418.
- Tejada-Simon, Maria V.; Zang, Ying C. Q.; Hong, Jian; Rivera, Victor M.; Zhang, Jingwu Z. (2003). "Cross-reactivity with myelin basic protein and human herpesvirus-6 in multiple sclerosis". Annals of Neurology. 53 (2): 189–97. doi:10.1002/ana.10425. PMID 12557285.
- Tait, A; Straus, S (2008). "Phosphorylation of U24 from Human Herpes Virus type 6 (HHV-6) and its potential role in mimicking myelin basic protein (MBP) in multiple sclerosis". FEBS Letters. 582 (18): 2685–8. doi:10.1016/j.febslet.2008.06.050. PMID 18616943.
- Knox, Konstance K.; Brewer, Joseph H.; Henry, James M.; Harrington, Daniel J.; Carrigan, Donald R. (2000). "Human Herpesvirus 6 and Multiple Sclerosis: Systemic Active Infections in Patients with Early Disease". Clinical Infectious Diseases. 31 (4): 894–903. doi:10.1086/318141. PMID 11049767.
- Pietilainen-Nicklen, J.; Virtanen, J (2014). "HHV-6-positivity in diseases with demyelination". Journal of Clinical Virology. 61 (2): 216–9. doi:10.1016/j.jcv.2014.07.006. PMID 25088617.
- Kawamura, Yoshiki; Sugata, Ken; Ihira, Masaru; Mihara, Takateru; Mutoh, Tatsuro; Asano, Yoshizo; Yoshikawa, Tetsushi (2011). "Different characteristics of human herpesvirus 6 encephalitis between primary infection and viral reactivation". Journal of Clinical Virology. 51 (1): 12–9. doi:10.1016/j.jcv.2011.02.002. PMID 21376661.
- Nora-Krukle, Z; Chapenko, S; Logina, I; Millers, A; Platkajis, A; Murovska, M (2011). "Human herpesvirus 6 and 7 reactivation and disease activity in multiple sclerosis". Medicina. 47 (10): 527–31. doi:10.3390/medicina47100075. PMID 22186115.
- Fukuda, K; Straus, SE; Hickie, I; Sharpe, MC; Dobbins, JG; Komaroff, A (1994). "The chronic fatigue syndrome: A comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group". Annals of Internal Medicine. 121 (12): 953–9. doi:10.7326/0003-4819-121-12-199412150-00009. PMID 7978722.
- Hickie, I.; Davenport, T; Wakefield, D; Vollmer-Conna, U; Cameron, B; Vernon, SD; Reeves, WC; Lloyd, A; Dubbo Infection Outcomes Study Group (2006). "Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: Prospective cohort study". BMJ. 333 (7568): 575. doi:10.1136/bmj.38933.585764.AE. PMC 1569956. PMID 16950834.
- Buchwald, D; Cheney, PR; Peterson, DL; Henry, B; Wormsley, SB; Geiger, A; Ablashi, DV; Salahuddin, SZ; et al. (1992). "A chronic illness characterized by fatigue, neurologic and immunologic disorders, and active human herpesvirus type 6 infection". Annals of Internal Medicine. 116 (2): 103–13. doi:10.7326/0003-4819-116-2-103. PMID 1309285.
- Ablashi, D.V; Eastman, H.B; Owen, C.B; Roman, M.M; Friedman, J; Zabriskie, J.B; Peterson, D.L; Pearson, G.R; Whitman, J.E (2000). "Frequent HHV-6 reactivation in multiple sclerosis (MS) and chronic fatigue syndrome (CFS) patients". Journal of Clinical Virology. 16 (3): 179–91. doi:10.1016/S1386-6532(99)00079-7. PMID 10738137.
- Reeves, W. C.; Stamey, F. R.; Black, J. B.; Mawle, A. C.; Stewart, J. A.; Pellett, P. E. (2000). "Human Herpesviruses 6 and 7 in Chronic Fatigue Syndrome: A Case-Control Study". Clinical Infectious Diseases. 31 (1): 48–52. doi:10.1086/313908. PMID 10913395.
- Nicolson, G. L.; Gan, R.; Haier, J. (2003). "Multiple co-infections (Mycoplasma, Chlamydia, human herpes virus-6) in blood of chronic fatigue syndrome patients: Association with signs and symptoms". APMIS. 111 (5): 557–66. doi:10.1034/j.1600-0463.2003.1110504.x. PMID 12887507.
- Patnaik, M.; Komaroff, A. L.; Conley, E.; Ojo-Amaize, E. A.; Peter, J. B. (1995). "Prevalence of IgM Antibodies to Human Herpesvirus 6 Early Antigen (p41/38) in Patients with Chronic Fatigue Syndrome". Journal of Infectious Diseases. 172 (5): 1364–7. doi:10.1093/infdis/172.5.1364. PMID 7594679.
- Secchiero, P.; Carrigan, D. R.; Asano, Y.; Benedetti, L.; Crowley, R. W.; Komaroff, A. L.; Gallo, R. C.; Lusso, P. (1995). "Detection of Human Herpesvirus 6 in Plasma of Children with Primary Infection and Immunosuppressed Patients by Polymerase Chain Reaction". Journal of Infectious Diseases. 171 (2): 273–80. doi:10.1093/infdis/171.2.273. PMID 7844362.
- Wagner, Mathias; Krueger, Gerhard; Ablashi, Dharam; Whitman, James (1996). "Chronic Fatigue Syndrome (CFS): A Critical Evaluation of Testing for Active Human Herpesvirus-6 (HHV-6) Infection". Journal of Chronic Fatigue Syndrome. 2 (4): 3–16. doi:10.1300/J092v02n04_02.
- Zorzenon, Marcella; Rukh, Gull; Botta, Giuseppe; Colle, Roberto; Barsanti, Laura; Ceccherini-Nelli, Luca (1996). "Active HHV-6 Infection in Chronic Fatigue Syndrome Patients from Italy". Journal of Chronic Fatigue Syndrome. 2: 3–12. doi:10.1300/J092v02n01_02.
- Koelle, David M.; Barcy, Serge; Huang, Meei‐Li; Ashley, Rhoda L.; Corey, Lawrence; Zeh, Judy; Ashton, Suzanne; Buchwald, Dedra (2002). "Markers of Viral Infection in Monozygotic Twins Discordant for Chronic Fatigue Syndrome". Clinical Infectious Diseases. 35 (5): 518–25. doi:10.1086/341774. PMID 12173124.
- Caselli, Elisabetta; Zatelli, Maria Chiara; Rizzo, Roberta; Benedetti, Sabrina; Martorelli, Debora; Trasforini, Giorgio; Cassai, Enzo; Degli Uberti, Ettore C.; et al. (October 2012). Moore, Patrick S (ed.). "Virologic and immunologic evidence supporting an association between HHV-6 and Hashimoto's thyroiditis". PLOS Pathogens. 8 (10): e1002951. doi:10.1371/journal.ppat.1002951. PMC 3464215. PMID 23055929.
- Silasi, Michelle (March 2013). "Viral invasion of the Amniotic Cavity (VIAC) in the Midtrimester of Pregnancy". American Journal of Reproductive Immunology. 69 (3): 195–196. doi:10.1111/aji.12073. PMID 23384234.
- Marci Roberto, Gentili Valentina, Bortolotti Daria, Lo Monte Giuseppe, Caselli Elisabetta, Bolzani Silvia, Rotola Antonella, Di Luca Dario, Rizzo Roberta (2016). "Presence of HHV-6A in Endometrial Epithelial Cells from Women with Primary Unexplained Infertility". PLOS One. 11 (7): e0158304. Bibcode:2016PLoSO..1158304M. doi:10.1371/journal.pone.0158304. PMC 4930213. PMID 27367597.CS1 maint: multiple names: authors list (link)
- Tamburro, Kristen; Yang, Dongmei; Poisson, Jessica; Fedoriw, Yuri; Roy, Debasmita; Lucas, Amy; Sin, Sang-Hoon; Malouf, Nadia; et al. (10 November 2012). "Vironome of Kaposi sarcoma associated herpesvirus-inflammatory cytokine syndrome in an AIDS patient reveals co-infection of human herpesvirus 8 and human herpesvirus 6A". Virology. 433 (1): 220–225. doi:10.1016/j.virol.2012.08.014. PMC 3505605. PMID 22925337.
- Parkin, Donald Maxwell (2006). "The global health burden of infection-associated cancers in the year 2002". International Journal of Cancer. 118 (12): 3030–44. doi:10.1002/ijc.21731. PMID 16404738.
- Oberacher-Velten, Isabel M.; Jonas, Jost B.; Jünemann, Anselm; Schmidt, Barbara (2004). "Bilateral optic neuropathy and unilateral tonic pupil associated with acute human herpesvirus 6 infection: A case report". Graefe's Archive for Clinical and Experimental Ophthalmology. 243 (2): 175–7. doi:10.1007/s00417-004-0986-8. PMID 15742213.
- Maslin, Jérôme; Bigaillon, Christine; Froussard, Françoise; Enouf, Vincent; Nicand, Elisabeth (2007). "Acute bilateral uveitis associated with an active human herpesvirus-6 infection". Journal of Infection. 54 (4): e237–40. doi:10.1016/j.jinf.2006.12.012. PMID 17303245.
- Ogata, Nahoko; Koike, Naoko; Yoshikawa, Tadanobu; Takahashi, Kanji (2011). "Human herpesvirus 6-associated uveitis with optic neuritis diagnosed by multiplex PCR". Japanese Journal of Ophthalmology. 55 (5): 502–5. doi:10.1007/s10384-011-0069-4. PMID 21814813.
- Li, Jin-Mei; Lei, Ding; Peng, Fang; Zeng, Yi-Jun; Li, Liang; Xia, Zeng-Liang; Xia, Xiao-Qiang; Zhou, Dong (2011). "Detection of human herpes virus 6B in patients with mesial temporal lobe epilepsy in West China and the possible association with elevated NF-κB expression". Epilepsy Research. 94 (1–2): 1–9. doi:10.1016/j.eplepsyres.2010.11.001. PMID 21256714.
- Noguchi, T.; Yoshiura, T.; Hiwatashi, A.; Togao, O.; Yamashita, K.; Nagao, E.; Uchino, A.; Hasuo, K.; et al. (2010). "CT and MRI Findings of Human Herpesvirus 6-Associated Encephalopathy: Comparison with Findings of Herpes Simplex Virus Encephalitis". American Journal of Roentgenology. 194 (3): 754–60. doi:10.2214/AJR.09.2548. PMID 20173155.
- Niehusmann, Pitt; Mittelstaedt, Tobias; Bien, Christian G.; Drexler, Jan F.; Grote, Alexander; Schoch, Susanne; Becker, Albert J. (2010). "Presence of human herpes virus 6 DNA exclusively in temporal lobe epilepsy brain tissue of patients with history of encephalitis". Epilepsia. 51 (12): 2478–83. doi:10.1111/j.1528-1167.2010.02741.x. PMID 21204811.
- Buyse, S.; Roque-Afonso, A.-M.; Vaghefi, P.; Gigou, M.; Dussaix, E.; Duclos-Vallee, J.-C.; Samuel, D.; Guettier, C. (2013). "Acute Hepatitis With Periportal Confluent Necrosis Associated With Human Herpesvirus 6 Infection in Liver Transplant Patients". American Journal of Clinical Pathology. 140 (3): 403–9. doi:10.1309/AJCP0FWI2XAHECBJ. PMID 23955460.
- Nakano, Kazushi; Nishinaka, Kazuko; Tanaka, Tatsuya; Ohshima, Atsushi; Sugimoto, Nakaba; Isegawa, Yuji (2009). "Detection and identification of U69 gene mutations encoded by ganciclovir-resistant human herpesvirus 6 using denaturing high-performance liquid chromatography". Journal of Virological Methods. 161 (2): 223–30. doi:10.1016/j.jviromet.2009.06.016. PMID 19559728.
- Shiley, Kevin; Blumberg, Emily (2010). "Herpes Viruses in Transplant Recipients: HSV, VZV, Human Herpes Viruses, and EBV". Infectious Disease Clinics of North America. 24 (2): 373–93. doi:10.1016/j.idc.2010.01.003. PMID 20466275.
External links
 Media related to Human herpesvirus 6 at Wikimedia Commons
Media related to Human herpesvirus 6 at Wikimedia Commons Data related to Human herpesvirus 6 at Wikispecies
Data related to Human herpesvirus 6 at Wikispecies