Alcohol intoxication
Alcohol intoxication, also known as drunkenness or alcohol poisoning,[1] is the negative behavior and physical effects due to the recent drinking of alcohol.[6][10] Symptoms at lower doses may include mild sedation and poor coordination.[3] At higher doses, there may be slurred speech, trouble walking, and vomiting.[3] Extreme doses may result in a respiratory depression, coma, or death.[3] Complications may include seizures, aspiration pneumonia, injuries including suicide, and low blood sugar.[3][4] Alcohol intoxication can lead to alcohol-related crime with perpetrators more likely to be intoxicated than victims.[11]
| Alcohol intoxication | |
|---|---|
| Other names | Drunkenness, acute alcohol poisoning, ethanol intoxication, acute alcohol intoxication[1][2] |
 | |
| The Drunkenness of Noah by Michelangelo, 1509 | |
| Specialty | Toxicology, psychiatry |
| Symptoms | Mild: Mild sedation, decreased coordination[3] Moderate: Slurred speech, trouble walking, vomiting[3] Severe: Decreased effort to breathe, coma[3] |
| Complications | Seizures, aspiration pneumonia, injuries, low blood sugar[3][4] |
| Usual onset | Over minutes to hours[5] |
| Duration | Several hours[5] |
| Causes | Ethanol (alcohol)[6] |
| Risk factors | Social environment, impulsivity, alcoholism[5][7] |
| Diagnostic method | Typically based on history of events and physical examination[6] |
| Differential diagnosis | Hepatic encephalopathy, Wernicke encephalopathy, methanol toxicity, meningitis, traumatic brain injury[6] |
| Treatment | Supportive care[6] |
| Frequency | Very common (especially in the Western world)[8] |
| Deaths | c. 2,200 per year (USA)[9] |
Alcohol intoxication typically begins after two or more alcoholic drinks.[5] Risk factors include a social situation where heavy drinking is common and a person having an impulsive personality.[5] Diagnosis is usually based on the history of events and physical examination.[6] Verification of events by witnesses may be useful.[6] Legally, alcohol intoxication is often defined as a blood alcohol concentration (BAC) of greater than 5.4–17.4 mmol/L (25–80 mg/dL or 0.025–0.080%).[12][13] This can be measured by blood or breath testing.[5] Alcohol is broken down in human body at a rate of about 3.3 mmol/L (15 mg/dL) per hour.[6]
Management of alcohol intoxication involves supportive care.[6] Typically this includes putting the person in the recovery position, keeping the person warm, and making sure breathing is sufficient.[4] Gastric lavage and activated charcoal have not been found to be useful.[6] Repeated assessments may be required to rule out other potential causes of a person's symptoms.[6]
Alcohol intoxication is very common, especially in the Western world.[8] Most people who drink alcohol have at some time been intoxicated.[5] In the United States acute intoxication directly results in about 2,200 deaths per year,[9] and indirectly more than 30,000 deaths per year.[5] Acute intoxication has been documented throughout history and alcohol remains one of the world's most widespread recreational drugs.[14][15] Some religions consider alcohol intoxication to be a sin.[5][16]
Alcohol intoxication symptoms

Alcohol intoxication is the negative health effects due to the recent drinking of ethanol (alcohol).[6] When severe it may become a medical emergency. Some effects of alcohol intoxication, such as euphoria and lowered social inhibition, are central to alcohol's desirability.[17]
Effect by alcohol level
| BAC (% by vol.) | SI units (mmol/l) | mg/dL | Behavior | Impairment |
|---|---|---|---|---|
| 0.001–0.029 | 0.22–6.3 | 1–29 |
|
|
| 0.030–0.059 | 6.5–12.8 | 30-59 |
|
|
| 0.060–0.099 | 13.0–21.5 | 60-99 |
| |
| 0.100–0.199 | 21.7–43.3 | 100-199 |
| |
| 0.200–0.299 | 43.4–64.9 | 200–299 |
|
|
| 0.300–0.399 | 65.1–86.6 | 300–399 |
|
|
| 0.400–0.500 | 86.80–108.5 | 400–500 |
|
|
| >0.50 | >108.5 | >500 |
|
Pathophysiology
Alcohol is metabolized by a normal liver at the rate of about 8 grams of pure ethanol per hour. 8 grams or 10 ml (0.34 US fl oz) is one British standard unit. An "abnormal" liver with conditions such as hepatitis, cirrhosis, gall bladder disease, and cancer is likely to result in a slower rate of metabolism.[19]
Ethanol is metabolised to acetaldehyde by alcohol dehydrogenase (ADH), which is found in many tissues, including the gastric mucosa. Acetaldehyde is metabolised to acetate by acetaldehyde dehydrogenase (ALDH), which is found predominantly in liver mitochondria. Acetate is used by the muscle cells to produce acetyl-CoA using the enzyme acetyl-CoA synthetase, and the acetyl-CoA is then used in the citric acid cycle.[20]
As drinking increases, people become sleepy, or fall into a stupor. After a very high level of consumption, the respiratory system becomes depressed and the person will stop breathing. Comatose patients may aspirate their vomit (resulting in vomitus in the lungs, which may cause "drowning" and later pneumonia if survived). CNS depression and impaired motor co-ordination along with poor judgment increases the likelihood of accidental injury occurring. It is estimated that about one-third of alcohol-related deaths are due to accidents and another 14% are from intentional injury.[21]
In addition to respiratory failure and accidents caused by effects on the central nervous system, alcohol causes significant metabolic derangements. Hypoglycaemia occurs due to ethanol's inhibition of gluconeogenesis, especially in children, and may cause lactic acidosis, ketoacidosis, and acute kidney injury. Metabolic acidosis is compounded by respiratory failure. Patients may also present with hypothermia.
Mechanism
In the past, alcohol was believed to be a non-specific pharmacological agent affecting many neurotransmitter systems in the brain.[22] However, molecular pharmacology studies have shown that alcohol has only a few primary targets. In some systems, these effects are facilitatory and in others inhibitory.
Among the neurotransmitter systems with enhanced functions are: GABAA,[23] 5-HT3 receptor agonism[24] (responsible for GABAergic (GABAA receptor PAM), glycinergic, and cholinergic effects), nicotinic acetylcholine receptors.[25]
Among those that are inhibited are: NMDA,[24] dihydropyridine-sensitive L-type Ca2+ channels[26] and G-protein-activated inwardly rectifying K+ channels.[27]
Alcohol is also converted to a lipid metabolite phosphatidylethanol by phospholipase D2 and this metabolite is shown to bind directly to and regulate ion channels.[28][29] The result of these direct effects is a wave of further indirect effects involving a variety of other neurotransmitter and neuropeptide systems, leading finally to the behavioural or symptomatic effects of alcohol intoxication.[22]
The order in which different types of alcohol are consumed ("Grape or grain but never the twain" and "Beer before wine and you'll feel fine; wine before beer and you'll feel queer") does not have any effect.[30]
GABAA receptors
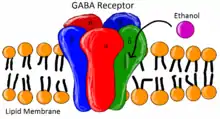
Many of the effects of activating GABAA receptors have the same effects as that of ethanol consumption. Some of these effects include anxiolytic, anticonvulsant, sedative, and hypnotic effects, cognitive impairment, and motor incoordination.[31] This correlation between activating GABAA receptors and the effects of ethanol consumption has led to the study of ethanol and its effects on GABAA receptors. It has been shown that ethanol does in fact exhibit positive allosteric binding properties to GABAA receptors. However, its effects are limited to pentamers containing the δ-subunit rather than the γ-subunit.[32] GABAA receptors containing the δ-subunit have been shown to be located exterior to the synapse and are involved with tonic inhibition rather than its γ-subunit counterpart, which is involved in phasic inhibition.[31] The δ-subunit has been shown to be able to form the allosteric binding site which makes GABAA receptors containing the δ-subunit more sensitive to ethanol concentrations, even to moderate social ethanol consumption levels (30mM).[33] While it has been shown by Santhakumar et al. that GABAA receptors containing the δ-subunit are sensitive to ethanol modulation, depending on subunit combinations receptors, could be more or less sensitive to ethanol.[34] It has been shown that GABAA receptors that contain both δ and β3-subunits display increased sensitivity to ethanol.[32] One such receptor that exhibits ethanol insensitivity is α3-β6-δ GABAA.[34] It has also been shown that subunit combination is not the only thing that contributes to ethanol sensitivity. Location of GABAA receptors within the synapse may also contribute to ethanol sensitivity.[31]
Diagnosis
Definitive diagnosis relies on a blood test for alcohol, usually performed as part of a toxicology screen. Law enforcement officers in the United States and other countries often use breathalyzer units and field sobriety tests as more convenient and rapid alternatives to blood tests.[35] There are also various models of breathalyzer units that are available for consumer use. Because these may have varying reliability and may produce different results than the tests used for law-enforcement purposes, the results from such devices should be conservatively interpreted.
Many informal intoxication tests exist, which, in general, are unreliable and not recommended as deterrents to excessive intoxication or as indicators of the safety of activities such as motor vehicle driving, heavy equipment operation, machine tool use, etc.
For determining whether someone is intoxicated by alcohol by some means other than a blood-alcohol test, it is necessary to rule out other conditions such as hypoglycemia, stroke, usage of other intoxicants, mental health issues, and so on. It is best if their behavior has been observed while the subject is sober to establish a baseline. Several well-known criteria can be used to establish a probable diagnosis. For a physician in the acute-treatment setting, acute alcohol intoxication can mimic other acute neurological disorders, or is frequently combined with other recreational drugs that complicate diagnosis and treatment.
Management
Acute alcohol poisoning is a medical emergency due to the risk of death from respiratory depression or aspiration of vomit if vomiting occurs while the person is unresponsive. Emergency treatment strives to stabilize and maintain an open airway and sufficient breathing, while waiting for the alcohol to metabolize. This can be done by removal of any vomit or, if the person is unconscious or has impaired gag reflex, intubation of the trachea.[36]
Other measures may include
- Treat low blood sugar, with intravenous sugar solutions as ethanol induced low blood sugar unresponsive to glucagon.
- Administer the vitamin thiamine to prevent Wernicke–Korsakoff syndrome, which can cause a seizure (more usually a treatment for chronic alcoholism, but in the acute context usually co-administered to ensure maximal benefit).
- Hemodialysis if the blood concentration is very high at >130 mmol/l (>600 mg/dL)[37]
- Provide oxygen therapy as needed via nasal cannula or non-rebreather mask.
- While the medication metadoxine may speed the breakdown of alcohol, use in alcohol intoxication requires further study as of 2017.[6][38] It is approved in a number of countries in Europe, as well as India and Brazil.[38]
Additional medication may be indicated for treatment of nausea, tremor, and anxiety.
Prognosis
A normal liver detoxifies the blood of alcohol over a period of time that depends on the initial level and the patient's overall physical condition. An abnormal liver will take longer but still succeeds, provided the alcohol does not cause liver failure.[39]
People having drunk heavily for several days or weeks may have withdrawal symptoms after the acute intoxication has subsided.[40]
A person consuming a dangerous amount of alcohol persistently can develop memory blackouts and idiosyncratic intoxication or pathological drunkenness symptoms.[41]
Long-term persistent consumption of excessive amounts of alcohol can cause liver damage and have other deleterious health effects.
Society and culture
Alcohol intoxication is a risk factor in some cases of catastrophic injury, in particular for unsupervised recreational activity. A study in the province of Ontario based on epidemiological data from 1986, 1989, 1992, and 1995 states that 79.2% of the 2,154 catastrophic injuries recorded for the study were preventable, of which 346 (17%) involved alcohol consumption.[42] The activities most commonly associated with alcohol-related catastrophic injury were snowmobiling (124), fishing (41), diving (40), boating (31) and canoeing (7), swimming (31), riding an all-terrain vehicle (24), and cycling (23).[42] These events are often associated with unsupervised young males, often inexperienced in the activity, and many result in drowning.[42] Alcohol use is also associated with unsafe sex.
Legal issues

Laws on drunkenness vary. In the United States, it is a criminal offense for a person to be drunk while driving a motorized vehicle, except in Wisconsin, where it is only a fine for the first offense.[43] It is also a criminal offense to fly an aircraft or (in some American states) to assemble or operate an amusement park ride while drunk.[44] Similar laws also exist in the United Kingdom and most other countries.
In some countries, it is also an offense to serve alcohol to an already-intoxicated person,[45] and, often, alcohol can be sold only by persons qualified to serve responsibly through alcohol server training.
The blood alcohol content (BAC) for legal operation of a vehicle is typically measured as a percentage of a unit volume of blood. This percentage ranges from 0.00% in Romania and the United Arab Emirates; to 0.05% in Australia, South Africa, Germany, Scotland and New Zealand (0.00% for underage individuals); to 0.08% in England and Wales, the United States (0.00% for underaged individuals) and Canada.[46]
The United States Federal Aviation Administration prohibits crew members from performing their duties within eight hours of consuming an alcoholic beverage, while under the influence of alcohol, or with a BAC greater than 0.04%.[47][48]
In the United States, the United Kingdom, and Australia, public intoxication is a crime (also known as "being drunk and disorderly" or "being drunk and incapable").[49]
In some countries, there are special facilities, sometimes known as "drunk tanks", for the temporary detention of persons found to be drunk.
Religious views
.jpg.webp)
Some religious groups permit the consumption of alcohol. Some permit consumption but prohibit intoxication, while others prohibit alcohol consumption altogether. Many Christian denominations such as Catholic, Orthodox, and Lutheran use wine as a part of the Eucharist and permit the drinking of alcohol but consider it sinful to become intoxicated.
In the Bible, the Book of Proverbs contains several chapters dealing with the bad effects of drunkenness and warning to stay away from intoxicating beverages. The book of Leviticus tells of Nadab and Abihu, Aaron the Priest's eldest sons, who were killed for serving in the temple after drinking wine, presumably while intoxicated. The book continues to discuss monasticism where drinking wine is prohibited. The story of Samson in the Book of Judges tells of a monk from the tribe of Dan who is prohibited from cutting his hair and drinking wine.[50] Romans 13:13–14,[51] 1 Corinthians 6:9–11, Galatians 5:19–21,[52] and Ephesians 5:18[53] are among a number of other Bible passages that speak against drunkenness. While Proverbs 31:4, warns against kings and rulers drinking wine and strong drink, Proverbs 31:6–7 promotes giving strong drink to the perishing and wine to those whose lives are bitter, to forget their poverty and troubles.[54]
Some Protestant Christian denominations prohibit the drinking of alcohol[55] based upon Biblical passages that condemn drunkenness,[50] but others allow moderate use of alcohol.[56] In some Christian groups, a small amount of wine is part of the rite of communion.
In the Church of Jesus Christ of Latter-day Saints, alcohol consumption is forbidden,[57] and teetotalism has become a distinguishing feature of its members. Jehovah's Witnesses allow moderate alcohol consumption among its members.
In the Qur'an,[58][59][60] there is a prohibition on the consumption of grape-based alcoholic beverages, and intoxication is considered as an abomination in the Hadith. Islamic schools of law (Madh'hab) have interpreted this as a strict prohibition of the consumption of all types of alcohol and declared it to be haraam ("forbidden"), although other uses may be permitted.[61]
In Buddhism, in general, the consumption of intoxicants is discouraged for both monastics and lay followers. Many followers of Buddhism observe a code of conduct known as the five precepts, of which the fifth precept is an undertaking to refrain from the consumption of intoxicating substances[62] (except for medical reasons).[63] In the bodhisattva vows of the Brahma Net Sūtra, observed by Mahāyāna Buddhist communities, distribution of intoxicants is likewise discouraged, as well as consumption.[64]
In the branch of Hinduism known as Gaudiya Vaishnavism, one of the four regulative principles forbids the taking of intoxicants, including alcohol.
In Judaism, in accordance with the biblical stance against drinking,[50] wine drinking was not permitted for priests and monks[65] The biblical command to sanctify the Sabbath day and other holidays has been interpreted as having three ceremonial meals which include drinking of wine, the Kiddush.[66][67] The Jewish marriage ceremony ends with the bride and groom drinking a shared cup of wine after reciting seven blessings, and according to western "Ashkenazi" traditions, after a fast day. But it has been customary and in many cases even mandated to drink moderately so as to stay sober, and only after the prayers are over.[68]
During the Seder night on Passover (Pesach) there is an obligation to drink 4 ceremonial cups of wine, while reciting the Haggadah. It has been assumed as the source for the wine drinking ritual at the communion in some Christian groups.[69] During Purim there is an obligation to become intoxicated, although, as with many other decrees, in many communities this has been avoided, by allowing sleep during the day to replace it.[70]
In the 1920s due to the new beverages law, a rabbi from the Reform Judaism movement proposed using grape-juice for the ritual instead of wine. Although refuted at first, the practice became widely accepted by orthodox Jews as well.[71]
At the Cave of the Patriarchs in Hebron—the Ibrahimi Mosque as it is called by the Muslims, the Jewish wine drinking rituals during weddings, the Sabbath day and holidays, are a cause for tension with the Muslims who unwillingly share the site under Israeli authority.[72]
Other animals
In the movie Animals are Beautiful People, an entire section was dedicated to showing many different animals including monkeys, elephants, hogs, giraffes, and ostriches, eating over-ripe marula tree fruit causing them to sway and lose their footing in a manner similar to human drunkenness.[73] Birds may become intoxicated with fermented berries and some die colliding with hard objects when flying under the influence.[74][75]
In elephant warfare, practiced by the Greeks during the Maccabean revolt and by Hannibal during the Punic wars, it has been recorded that the elephants would be given wine before the attack, and only then would they charge forward after being agitated by their driver.[76]
It is a regular practice to give small amounts of beer to race horses in Ireland. Ruminant farm animals have natural fermentation occurring in their stomach, and adding alcoholic beverages in small amounts to their drink will generally do them no harm, and will not cause them to become drunk.
Alcoholic beverages are extremely harmful to dogs,[77] and often for reasons of additives such as xylitol, an artificial sweetener in some mixers. Dogs can absorb ethyl alcohol in dangerous amounts through their skin as well as through drinking the liquid or consuming it in foods. Even fermenting bread dough can be dangerous to dogs.[78]
See also
References
- Garfunkel, Lynn C.; Kaczorowski, Jeffrey; Christy, Cynthia (2007). Pediatric Clinical Advisor E-Book: Instant Diagnosis and Treatment. Elsevier Health Sciences. p. 13. ISBN 9780323070584.
- Gupta, P. K. (2016). Fundamentals of Toxicology: Essential Concepts and Applications. Academic Press. ISBN 978-0-12-805403-1.
Alcohol poisoning presents in two forms, acute and chronic. However, these are most often referred to as alcohol intoxication and alcohol addiction respectively.
- "Alcohol Toxicity and Withdrawal". Merck Manuals Professional Edition. Retrieved 24 May 2018.
- "Alcohol poisoning". nhs.uk. 2017-10-17. Retrieved 24 May 2018.
- American Psychiatric Association (2013), Diagnostic and Statistical Manual of Mental Disorders (5th ed.), Arlington: American Psychiatric Publishing, pp. 497–499, ISBN 978-0890425558
- Jung, YC; Namkoong, K (2014). Alcohol: intoxication and poisoning – diagnosis and treatment. Handbook of Clinical Neurology. 125. pp. 115–21. doi:10.1016/B978-0-444-62619-6.00007-0. ISBN 9780444626196. PMID 25307571.
- "Alcohol use disorder – Symptoms and causes". Mayo Clinic. Retrieved 26 November 2019.
- Vonghia, L; Leggio, L; Ferrulli, A; Bertini, M; Gasbarrini, G; Addolorato, G; Alcoholism Treatment Study, Group. (December 2008). "Acute alcohol intoxication". European Journal of Internal Medicine. 19 (8): 561–7. doi:10.1016/j.ejim.2007.06.033. PMID 19046719.
- Kanny, D; Brewer, RD; Mesnick, JB; Paulozzi, LJ; Naimi, TS; Lu, H (9 January 2015). "Vital signs: alcohol poisoning deaths – United States, 2010–2012". MMWR. Morbidity and Mortality Weekly Report. 63 (53): 1238–42. PMC 4646044. PMID 25577989.
- "Acute intoxication". WHO. Retrieved 24 May 2018.
- Sung, Hung-En (2016), "Alcohol and Crime", The Blackwell Encyclopedia of Sociology, American Cancer Society, pp. 1–2, doi:10.1002/9781405165518.wbeosa039.pub2, ISBN 978-1-4051-6551-8
- "Ethanol Level: Reference Range, Interpretation, Collection and Panels". Medscape. 22 April 2018. Retrieved 24 May 2018.
- Canfield, DV; Dubowski, KM; Cowan, M; Harding, PM (January 2014). "Alcohol Limits and Public Safety". Forensic Science Review. 26 (1): 9–22. PMID 26226968.
- Belenko, Steven; Spohn, Cassia (2014). Drugs, Crime, and Justice. SAGE Publications. p. PT21. ISBN 9781483355429.
- Martin, Scott C. (2014). The SAGE Encyclopedia of Alcohol: Social, Cultural, and Historical Perspectives. SAGE Publications. p. PT1382. ISBN 9781483374383.
- Kolig, Erich (2012). Conservative Islam: A Cultural Anthropology. Lexington Books. p. 101. ISBN 9780739174258.
- Dudley, Robert, 1961– (May 2014). The drunken monkey : why we drink and abuse alcohol. Berkeley. ISBN 978-0-520-95817-3. OCLC 869457130.CS1 maint: multiple names: authors list (link)
- A hybridizing of effects as described at Alcohol's Effects Archived May 5, 2007, at the Wayback Machine from Virginia Tech and Federal Aviation Regulation (CFR) 91.17: Alcohol and Flying (hosted on FlightPhysical.com)
- "How long does alcohol stay in your blood?". NHS Choices. 2018-06-26.
- Smith, C., Marks, Allan D., Lieberman, Michael, 2005, Marks' Basic Medical Biochemistry: A Clinical Approach, 2nd ed., Lippincott Williams & Wilkins, USA, p. 458
- The World Health Organisation (2007) Alcohol and Injury in Emergency Departments
- Vengeliene, V; Bilbao, A; Molander, A; Spanagel, R (2008). "Neuropharmacology of alcohol addiction". British Journal of Pharmacology. 154 (2): 299–315. doi:10.1038/bjp.2008.30. PMC 2442440. PMID 18311194.
- Mihic, S. John; Ye, Qing; Wick, Marilee J.; Koltchine, Vladimir V.; Krasowski, Matthew D.; Finn, Suzanne E.; Mascia, Maria Paola; Valenzuela, C. Fernando; et al. (1997). "Sites of alcohol and volatile anaesthetic action on GABA(A) and glycine receptors". Nature. 389 (6649): 385–389. Bibcode:1997Natur.389..385M. doi:10.1038/38738. PMID 9311780. S2CID 4393717.
- Lovinger, D. M., David M (1999). "5-HT3 receptors and the neural action of alcohols: An increasingly exciting topic". Neurochemistry International. 35 (2): 125–130. doi:10.1016/S0197-0186(99)00054-6. PMID 10405996. S2CID 1391767.
- Narahashi, Toshio; Aistrup, Gary L; Marszalec, William; Nagata, Keiichi (1999). "Neuronal nicotinic acetylcholine receptors: A new target site of ethanol". Neurochemistry International. 35 (2): 131–141. doi:10.1016/S0197-0186(99)00055-8. PMID 10405997. S2CID 40991187.
- Wang, X; Wang, G; Lemos, JR; Treistman, SN (1994). "Ethanol directly modulates gating of a dihydropyridine-sensitive Ca2+ channel in neurohypophysial terminals". The Journal of Neuroscience. 14 (9): 5453–5460. doi:10.1523/JNEUROSCI.14-09-05453.1994. PMC 6577079. PMID 7521910.
- Kobayashi, Toru; Ikeda, Kazutaka; Kojima, Hiroshi; Niki, Hiroaki; Yano, Ryoji; Yoshioka, Tohru; Kumanishi, Toshiro (1999). "Ethanol opens G-protein activated inwardly rectifying K+ channels". Nature Neuroscience. 2 (12): 1091–1097. doi:10.1038/16019. PMID 10570486. S2CID 28730710.
- Chung, HW; Petersen, EN; Cabanos, C; Murphy, KR; Pavel, MA; Hansen, AS; Ja, WW; Hansen, SB (18 January 2019). "A Molecular Target for an Alcohol Chain-Length Cutoff". Journal of Molecular Biology. 431 (2): 196–209. doi:10.1016/j.jmb.2018.11.028. PMC 6360937. PMID 30529033.
- Robinson, CV; Rohacs, T; Hansen, SB (September 2019). "Tools for Understanding Nanoscale Lipid Regulation of Ion Channels". Trends in Biochemical Sciences. 44 (9): 795–806. doi:10.1016/j.tibs.2019.04.001. PMC 6729126. PMID 31060927.
- Köchling, Jöran; Geis, Berit; Wirth, Stefan; Hensel, Kai O (February 2019). "Grape or grain but never the twain? A randomized controlled multiarm matched-triplet crossover trial of beer and wine". The American Journal of Clinical Nutrition. 109 (2): 345–352. doi:10.1093/ajcn/nqy309. PMC 6410559. PMID 30753321.
- Kumar, Sandeep; Porcu, Patrizia; Werner, David; Matthews, Douglas; Diaz-Granados, Jamie; Helfand, Rebecca; Morrow, Leslie (2009). "The role of GABAA receptors in the acute and chronic effects of ethanol: a decade of progress". Psychopharmacology. 205 (4): 529–64. doi:10.1007/s00213-009-1562-z. PMC 2814770. PMID 19455309.
- Santhakumar, Vijayalakshmi; Wallner, Martin; Otis, Thomas (2007). "Ethanol acts directly on extrasynaptic subtypes of GABAA receptors to increase tonic inhibition". Alcohol. 41 (3): 211–221. doi:10.1016/j.alcohol.2007.04.011. PMC 2040048. PMID 17591544.
- Wallner, Martin; Hanchar, Jacob; Olsen, Richard (2003). "Ethanol enhances alpha 4 beta 3 delta and alpha 6 beta 3 delta gamma-aminobutyric acid type A receptors at low concentrations known to affect humans". Proceedings of the National Academy of Sciences of the United States of America. 100 (25): 15218–15223. doi:10.1073/pnas.2435171100. PMC 299963. PMID 14625373.
- Baur, Roland; Kaur, Kuldeep; Sigel, Erwin (2009). "Structure of α6β3δ GABAA receptors and their lack of ethanol sensitivity". Journal of Neurochemistry. 111 (5): 1172–1181. doi:10.1111/j.1471-4159.2009.06387.x. PMID 19765192. S2CID 10577529.
- "Random breath testing – Data by country". apps.who.int. Retrieved 25 June 2018.
- Devi G.; Castro V. J.; Huitink J.; Buitelaar D.; Kosten T.; O'Connor P. (2003). "Management of Drug and Alcohol Withdrawal". NEJM. 349 (4): 405–407. doi:10.1056/NEJM200307243490420. PMID 12878752.
- Adinoff, B.; Bone, G. H.; Linnoila, M. (May 1988). "Acute ethanol poisoning and the ethanol withdrawal syndrome". Medical Toxicology. 3 (3): 172–196. doi:10.1007/BF03259881. PMID 3041244. S2CID 35315540.
- Goh, ET; Morgan, MY (April 2017). "Review article: pharmacotherapy for alcohol dependence – the why, the what and the wherefore" (PDF). Alimentary Pharmacology & Therapeutics. 45 (7): 865–882. doi:10.1111/apt.13965. PMID 28220511. S2CID 5431337.
- Morgan TR (2003). "Management of alcoholic hepatitis". Drug and Therapeutics Bulletin. 41 (2): 49–52. doi:10.1136/dtb.2003.41749. PMC 3099359. PMID 21960817.
- DeBellis R.; Smith B. S.; Choi S.; Malloy M. (2005). "Management of Delirium Tremens". J Intensive Care Med. 20 (3): 164–173. doi:10.1177/0885066605275353. PMID 15888905. S2CID 31848749.
- Gelder, M., Mayou, R. and Geddes, J. 2005. Psychiatry. 3rd ed. New York: Oxford. pp. 186.
- Tator, Charles H., ed. (2008). Catastrophic Injuries in Sports and Recreation: Causes and Prevention: A Canadian Study (2 ed.). University of Toronto Press. ISBN 9780802089670.
- "Wisconsin Legislature: Chapter 346". wisconsin.gov.
- Texas Penal Code § 49.065 Archived 2011-09-26 at the Wayback Machine
- "Camden Council: Booze license suspended after selling alcohol to drunk customers". camden.gov.uk. Archived from the original on 2009-01-11. Retrieved 2009-01-08.
- "Drinking and Driving". icap.org. Archived from the original on 2008-07-02.
- "Federal Aviation Regulation Sec. 1.1 – General definitions". risingup.com.
- "FAR Part 91 Sec. 91.17 effective as of 07/21/2006". faa.gov.
- "Licensing Act 1872". Acts of the United Kingdom Parliament. 1872. 1872-08-10. Archived from the original on 2012-08-05. Retrieved 2010-05-08.
- Biblical examples referencing intoxication: "Proverbs 23:21". Net.bible.org. Archived from the original on 2009-06-20. Retrieved 2009-11-03., "Isaiah 28:1". Net.bible.org. Archived from the original on 2009-06-20. Retrieved 2009-11-03., "Habakkuk 2:15". Net.bible.org. Archived from the original on 2009-06-20. Retrieved 2009-11-03.
- "Romans 13:13–14".
- "Galatians 5:19–21".
- "Ephesians 5:18".
- "Proverbs 31: 4–7 NASB—It is not for kings, O Lemuel, It is". Bible Gateway.
- "On Alcohol Use in America". SBC Resolutions. Southern Baptist Convention. June 2006. Retrieved 7 June 2013.
- "Frequently Asked Questions: Alcohol". LCMS Views – Contemporary Issues. Lutheran Church–Missouri Synod. p. 3. Retrieved 7 June 2013.
- "Doctrine and Covenants 89".
- "Qur'an: 4:43". Usc.edu. Archived from the original on 2010-12-04. Retrieved 2010-12-04.
- "Qur'an: 2:19". Usc.edu. Archived from the original on 4 December 2010. Retrieved 2010-12-04.
- "Cmje". usc.edu. Archived from the original on 2010-12-04. Retrieved 2010-12-04.
- Yilmaz, Ihsan (2004) [2005-01-31]. "Post-Modern Muslim Legality and its Consequences". Muslim Laws, Politics And Society In Modern Nation States: Dynamic Legal Pluralisms In England, Turkey And Pakistan. Ashgate Publishing. p. 158. ISBN 978-0-7546-4389-0.
- Gwynne, Paul (2017). "The Buddhist Pancasila". World Religions in Practice: A Comparative Introduction. John Wiley & Sons. ISBN 978-1-118-97227-4.
- Gombrich, Richard F. (1995). Buddhist Precept and Practice: Traditional Buddhism in the Rural Highlands of Ceylon. Kegan Paul, Trench and Company. p. 298. ISBN 978-0-7103-0444-5.
- Benn, James A. (2005). "Buddhism, Alcohol, and Tea in Medieval China". In Sterckx, R. (ed.). Of Tripod and Palate: Food, Politics, and Religion in Traditional China. Springer Nature. p. 226. ISBN 978-1-4039-7927-8.
- The Talmudic decree set a schedule according to which the priests would take turns staying sober. The practice of becoming a 'biblical' monk, is discussed in a full tractate of the Mishna and Talmud. The Talmud tells of a family 'the sons of Reichab' who never drank wine, although it is not clear if this is considered good or bad.
- The Kiddush is recited today only in the opening meal on Friday night and the main meal during the day. See On the mystery of the missing Kiddush during the third Sabbath meal Ruth Foichtwanger Segel, Shabbat Magazine, August 21, 2016 (Hebrew, Makor Rishon website)
- The Pharisees, avoiding the Zadokites' temple-based rituals, had installed many ceremonies which in a way change or contradict the literal meaning of the biblical protocol. These include the ceremony of lighting candles which stay lit during the Sabbath day, eating hot food from a fire lit previously, starting the Sabbath rituals on the night before, and the drinking of wine with the Sabbath meal. See Qimron Sabbath Laws Vered Noam, Department of Hebrew Culture Studies, Tel Aviv University (Dead Sea Discoveries Archived 2017-01-31 at the Wayback Machine, Brill Institute)
- Menachem Posner: What is Judaism's take on alcohol consumption? on Chabad.org
- Was Jesus' last supper a Seder? Jonathan Klawans, January 7, 2014 (Biblical Archaeology organization's website)
- The Babylonian Talmud says in Megillah 7b that "Rava said: A person is obligated to become intoxicated on Purim until he is unaware of the difference between 'Cursed be Haman' and 'Blessed be Mordechai.'" This is taken to mean that on the Jewish festival of Purim one is commanded to drink alcohol to the point of intoxication. See Yanki Tauber: Are Jews actually supposed to get drunk on Purim? Chabad.org (referring to the Talmudic tractate Megillah (7b)).
- Using grape juice for Kiddush (Torahlab website)
- Hebron: Jews and Palestinians share holy site begrudgingly, Daniel Estrin, November 10, 2015 (Public Radio International website)
- Drunken animals scene (YouTube)
- Katz, Brigit (4 October 2018). "Birds Are Acting Erratically in Minnesota. Blame It on the Alcohol". Smithsonian. Retrieved 5 October 2018.
- Kinde, Hailu; et al. (July 2012). "Strong circumstantial evidence for ethanol toxicosis in Cedar Waxwings (Bombycilla cedrorum)". Journal of Ornithology. 153 (3): 995–998. doi:10.1007/s10336-012-0858-7. S2CID 15546534.
- Hannibal's superweapon: The war elephant (HistoryThings.com website)
- https://www.akc.org/expert-advice/vets-corner/is-alcohol-dangerous-for-dogs/
- https://wagwalking.com/condition/alcohol-poisoning
Bibliography
- Bales, Robert F. "Attitudes toward Drinking in the Irish Culture". In: Pittman, David J. and Snyder, Charles R. (Eds.) Society, Culture and Drinking Patterns. New York: Wiley, 1962, pp. 157–187.
- Gentry, Kenneth L., Jr., God Gave Wine: What the Bible Says about Alcohol. Lincoln, Calif.: Oakdown, 2001.
- Rorabaugh, W.J. "The Alcoholic Republic," Chapter 2 & 5, Oxford University Press.
- Sigmund, Paul. St. Thomas Aquinas On Politics and Ethics. W.W. Norton & Company, Inc, 1988, p. 77.
- Walton, Stuart. Out of It. A Cultural History of Intoxication. Penguin Books, 2002. ISBN 0-14-027977-6.
External links
| Classification | |
|---|---|
| External resources |
| Wikisource has the text of the 1911 Encyclopædia Britannica article Drunkenness. |
- Alcohol overdose: NIAAA
- Alcohol poisoning: NHS Choices