CYP2C19
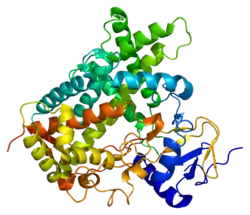
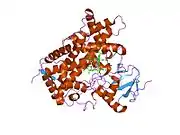
Cytochrome P450 2C19 (abbreviated CYP2C19) is an enzyme protein. It is a member of the CYP2C subfamily of the cytochrome P450 mixed-function oxidase system. This subfamily includes enzymes that catalize metabolism of xenobiotics, including some proton pump inhibitors and antiepileptic drugs. In humans, it is the CYP2C19 gene that encodes the CYP2C19 protein.[3][4] CYP2C19 is a liver enzyme that acts on at least 10% of drugs in current clinical use,[5] most notably the antiplatelet treatment clopidogrel (Plavix), drugs that treat pain associated with ulcers, such as omeprazole, antiseizure drugs such as mephenytoin, the antimalarial proguanil, and the anxiolytic diazepam.[6]
CYP2C19 has been annotated as (R)-limonene 6-monooxygenase and (S)-limonene 6-monooxygenase in UniProt.
Function
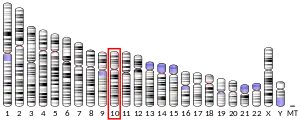
The gene encodes a member of the cytochrome P450 superfamily of enzymes. Enzymes in the CYP2C subfamily, including CYP2C19, account for approximately 20% of cytochrome P450 in the adult liver.[7] These proteins are monooxygenases that catalyze many reactions involved in drug metabolism and synthesis of cholesterol, steroids and other lipids. This protein localizes to the endoplasmic reticulum and is known to metabolize many drugs. Polymorphism within this gene is associated with variable ability to metabolize drugs. The gene is located within a cluster of cytochrome P450 genes on chromosome no.10 arm q24.[8]
CYP2C19 also possesses epoxygenase activity: it is one of the principal enzymes responsible for attacking various long-chain polyunsaturated fatty acids at their double (i.e. alkene) bonds to form epoxide products that act as signaling agents. It metabolizes:
- arachidonic acid to various epoxyeicosatrienoic acids (also termed EETs);
- linoleic acid to 9,10-epoxy octadecaenoic acids (also termed vernolic acid, linoleic acid 9:10-oxide, or leukotoxin) and 12,13-epoxy-octadecaenoic (also termed coronaric acid, linoleic acid 12,13-oxide, or isoleukotoxin);
- docosahexaenoic acid to various epoxydocosapentaenoic acids (also termed EDPs); and
- eicosapentaenoic acid to various epoxyeicosatetraenoic acids (also termed EEQs).[9][10][11]
Along with CYP2C19, CYP2C8, CYP2C9, CYP2J2, and possibly CYP2S1 are the main producers of EETs and, very likely EEQs, EDPs, and the epoxides of linoleic acid.[10][12]
Pharmacogenomics
Pharmacogenomics is a study that analyzes how an individual's genetic makeup affects the response to drugs of this individual. There are many common genetic variations that affect the expression of the CYP2C19 gene, which in turn influence the enzyme activity in the metabolic pathways of those drugs in which this enzyme is involved.
The Pharmacogene Variation Consortium keeps the Human CYP Allele Nomenclature Database and assigns labels to known polymorphsms that affect drug response. A label consists of an asterisk (*) character followed by a number. The most common variant (also called wild type) has CYP2C19*1 label. The variant genotypes of CYP2C19*2 (NM_000769.2:c.681G>A; p.Pro227Pro; rs4244285), CYP2C19*3 (NM_000769.2:c.636G>A; p.Trp212Ter; rs4986893) and CYP2C19*17 (NM_000769.2:c.-806C>T; rs12248560)[13] are major factors attributed to interindividual differences in the pharmacokinetics and response to CYP2C19 substrates.
CYP2C19*2 and *3 (loss-of-function alleles) are associated with diminished enzyme activity,[14][15] whereas CYP2C19*17 (gain-of-function allele) results in increased activity.[16] These three variant alleles are recommended by the Working Group of the Association for Molecular Pathology Clinical Practice Committee to be included in the minimal clinical pharmacogenomic testing panel, called tier 1. The extended panel of variant alleles, called tier 2, additionally includes the following CYP2C19 alleles: *4.001 (*4A), *4.002 (*4B), *5, *6, *7, *8, *9, *10, and *35, all of them associated with diminished enzyme activity. Although these tier 2 alleles are included in many platforms, they were not included in the tier 1 recommendations because of low minor allele frequency (which can result in an increase of false-positive results), less well-characterized impact on CYP2C19 function, or a lack of reference materials. To meet the need for publicly available characterized reference materials, the Centers for Disease Control and Prevention, in partnership with the clinical testing community, established the Genetic Testing Reference Material Program. Its goal is to improve the supply of publicly available and well-characterized genomic DNA that can be used as reference materials for proficiency testing, quality control, test development/validation, and research studies.[13]
The allele frequencies of CYP2C19*2 and *3 are significantly higher in Chinese populations than in European or African populations,[17] and are found at approximately 3–5% of European and 15–20% of Asian populations.[18][19] In a study of 2.29 million direct-to-consumer genetics research participants, the overall frequencies of *2, *3, and *17 were 15.2%, 0.3%, and 20.4%, respectively, but varied by ethnicity. The most common variant diplotypes were *1/*17 at 26% and *1/*2 at 19.4%. The less common *2/*17, *17/*17 and *2/*2 genotypes occurred at 6.0%, 4.4%, and 2.5%, respectively. Overall, 58.3% of participants had at least one increased-function or no-function CYP2C19 allele.[20]
CYP2C19 is involved in processing or metabolizing at least 10% of commonly prescribed drugs.[21] Variations to the enzyme can have a wide range of impacts to drug metabolism. In patients with an abnormal CYP2C19 variant certain benzodiazepines should be avoided, such as diazepam (Valium), lorazepam (Ativan), oxazepam (Serax), and temazepam (Restoril).[22] Other categories of drugs impacted by modified CYP2C19 include proton pump inhibitors, anticonvulsants, hypnotics, sedatives, antimalarial drugs, and antiretroviral drugs.[21]
On the basis of their ability to metabolize (S)-mephenytoin or other CYP2C19 substrates, individuals can be classified as ultrarapid metabolizers (UM), extensive metabolizers (EM) or poor metabolizers (PM).[19][23] In the case of proton pump inhibitors, PMs exhibit a drug exposure that is 3 to 13 times higher than that of EMs.[24] Loss-of-function alleles, CYP2C19*2 and CYP2C19*3 (and other, which are the subject of ongoing research) predict PMs,[19] and the gain-of-function CYP2C19*17 allele predicts UMs.[21]
Although the amount of CYP2C19 enzyme produced by the *17 allele is greater than of the *1 allele,[25] whether the carriers of the *17 allele experience any significant difference in response to drugs comparing to the wild-type, is a topic of ongoing research, studies show varying results.[23][26] Some studies have found that the *17 variant's effect on the metabolism of omeprazole, pantoprazole, escitalopram, sertraline, voriconazole, tamoxifen and clopidogrel[27] is modest, particularly compared to the impact of loss-of-function alleles (*2, *3), therefore, in case of these medications, the EM designation is sometimes applied instead of the UM classification. For example, carriers of the *17 allele did not demonstrate different gastric pH comparing to *1 after taking the proton pump inhibitor omeprazole, a CYP2C19 substrate.[23] Other studies concluded that the *17 allele seems to be the factor responsible for lower response to some drugs, even at higher doses, for example, to escitalopram for symptom remission in major depressive disorder patients.[26] CYP2C19*17 carrier status is significantly associated with enhanced response to clopidogrel and an increased risk of bleeding; the highest risk was observed for CYP2C19*17 homozygous patients.[28][29] A study have found that escitalopram serum concentration was 42% lower in patients homozygous for CYP2C19*17.[30] An important limitation of all these studies is the single-gene analysis, since most drugs that are metabolized by CYP2C19 are also metabolized by CYP2D6 and CYP3A4 enzymes. Besides that, other genes are involved in drug response, for example, escitalopram is transported by P-glycoprotein, encoded by the ABCB1 gene. In order for the studies on CYP2C19*17 to be conclusive, the differences in other genes that affect drug response have to be excluded.[26] The prevalence of the CYP2C19*17 variant is less than 5% in Asian populations and is approximately four times higher in European and African populations.[23]
The alleles CYP2C19*2 and *3 may reduce the efficacy of clopidogrel (Plavix), an antiplatelet medication. The basis for this reduced effect of clopidogrel in patients who have a gene of reduced activity may seem somewhat paradoxical, but can be understood as follows. Clopidogrel is administered as a “prodrug”, that is, a drug that is inactive when taken, and then depends on the action of an enzyme in the body in order to be activated. In patients who have a gene of reduced activity, clopidogrel may not be metabolized to its biologically active form and therefore not achieve pharmacological effect in the body. The relative risk of major cardiac events among patients treated with clopidogrel is 1.53 to 3.69 times higher for carriers of CYP2C19*2 and CYP2C19*3 compared with non-carriers.[31]
Ligands
The following is a table of selected substrates, inducers and inhibitors of CYP2C19. Where classes of agents are listed, there may be exceptions within the class.
Inhibitors of CYP2C19 can be classified by their potency, such as:
- Strong being one that causes at least a 5-fold increase in the plasma AUC values, or more than 80% decrease in clearance of substrates.[32]
- Moderate being one that causes at least a 2-fold increase in the plasma AUC values, or 50-80% decrease in clearance of substrates.[32]
- Weak being one that causes at least a 1.25-fold but less than 2-fold increase in the plasma AUC values, or 20-50% decrease in clearance of substrates.[32]
| Substrates | Inhibitors | Inducers |
|---|---|---|
|
|
|
See also
References
- GRCh38: Ensembl release 89: ENSG00000165841 - Ensembl, May 2017
- "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- Romkes M, Faletto MB, Blaisdell JA, Raucy JL, Goldstein JA (April 1991). "Cloning and expression of complementary DNAs for multiple members of the human cytochrome P450IIC subfamily". Biochemistry. 30 (13): 3247–55. doi:10.1021/bi00227a012. PMID 2009263.
- Gray IC, Nobile C, Muresu R, Ford S, Spurr NK (July 1995). "A 2.4-megabase physical map spanning the CYP2C gene cluster on chromosome 10q24". Genomics. 28 (2): 328–32. doi:10.1006/geno.1995.1149. PMID 8530044.
- "CYP2C19 gene". NIH Genetics Home Reference. Retrieved 6 September 2017.
- "Cytochrome P450 2C19 (CYP2C19) Genotype". Mayo Medical Laboratories. June 2013. Archived from the original on 15 April 2016. Retrieved 11 November 2014.
- Koukouritaki SB, Manro JR, Marsh SA, Stevens JC, Rettie AE, McCarver DG, Hines RN (March 2004). "Developmental expression of human hepatic CYP2C9 and CYP2C19". The Journal of Pharmacology and Experimental Therapeutics. 308 (3): 965–74. doi:10.1124/jpet.103.060137. PMID 14634042. S2CID 14838446.
- "Entrez Gene: CYP2C19 cytochrome P450, family 2, subfamily C, polypeptide 19". National Center for Biotechnology Information. Retrieved 30 November 2020.
This gene encodes a member of the cytochrome P450 superfamily of enzymes. The cytochrome P450 proteins are monooxygenases which catalyze many reactions involved in drug metabolism and synthesis of cholesterol, steroids and other lipids. This protein localizes to the endoplasmic reticulum and is known to metabolize many xenobiotics, including the anticonvulsive drug mephenytoin, omeprazole, diazepam and some barbiturates. Polymorphism within this gene is associated with variable ability to metabolize mephenytoin, known as the poor metabolizer and extensive metabolizer phenotypes. The gene is located within a cluster of cytochrome P450 genes on chromosome 10q24.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - Fleming I (October 2014). "The pharmacology of the cytochrome P450 epoxygenase/soluble epoxide hydrolase axis in the vasculature and cardiovascular disease". Pharmacological Reviews. 66 (4): 1106–40. doi:10.1124/pr.113.007781. PMID 25244930.
- Wagner K, Vito S, Inceoglu B, Hammock BD (October 2014). "The role of long chain fatty acids and their epoxide metabolites in nociceptive signaling". Prostaglandins & Other Lipid Mediators. 113–115: 2–12. doi:10.1016/j.prostaglandins.2014.09.001. PMC 4254344. PMID 25240260.
- Fischer R, Konkel A, Mehling H, Blossey K, Gapelyuk A, Wessel N, von Schacky C, Dechend R, Muller DN, Rothe M, Luft FC, Weylandt K, Schunck WH (June 2014). "Dietary omega-3 fatty acids modulate the eicosanoid profile in man primarily via the CYP-epoxygenase pathway". Journal of Lipid Research. 55 (6): 1150–64. doi:10.1194/jlr.M047357. PMC 4031946. PMID 24634501.
- Spector AA, Kim HY (April 2015). "Cytochrome P450 epoxygenase pathway of polyunsaturated fatty acid metabolism". Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids. 1851 (4): 356–65. doi:10.1016/j.bbalip.2014.07.020. PMC 4314516. PMID 25093613.
- Pratt VM, Del Tredici AL, Hachad H, Ji Y, Kalman LV, Scott SA, Weck KE (May 2018). "Recommendations for Clinical CYP2C19 Genotyping Allele Selection: A Report of the Association for Molecular Pathology". The Journal of Molecular Diagnostics. 20 (3): 269–276. doi:10.1016/j.jmoldx.2018.01.011. PMID 29474986.
- Ibeanu, G. C.; Goldstein, J. A.; Meyer, U.; Benhamou, S.; Bouchardy, C.; Dayer, P.; Ghanayem, B. I.; Blaisdell, J. (1998). "Identification of new human CYP2C19 alleles (CYP2C19*6 and CYP2C19*2B) in a Caucasian poor metabolizer of mephenytoin". The Journal of Pharmacology and Experimental Therapeutics. 286 (3): 1490–5. PMID 9732415.
- Fukushima-Uesaka, H.; Saito, Y.; Maekawa, K.; Ozawa, S.; Hasegawa, R.; Kajio, H.; Kuzuya, N.; Yasuda, K.; Kawamoto, M.; Kamatani, N.; Suzuki, K.; Yanagawa, T.; Tohkin, M.; Sawada, J. (2005). "Genetic variations and haplotypes of CYP2C19 in a Japanese population". Drug Metabolism and Pharmacokinetics. 20 (4): 300–7. doi:10.2133/dmpk.20.300. PMID 16141610.
- Sim, S. C.; Risinger, C.; Dahl, M. L.; Aklillu, E.; Christensen, M.; Bertilsson, L.; Ingelman-Sundberg, M. (2006). "A common novel CYP2C19 gene variant causes ultrarapid drug metabolism relevant for the drug response to proton pump inhibitors and antidepressants". Clinical Pharmacology and Therapeutics. 79 (1): 103–13. doi:10.1016/j.clpt.2005.10.002. PMID 16413245. S2CID 20989576.
- Wedlund PJ (September 2000). "The CYP2C19 enzyme polymorphism". Pharmacology. 61 (3): 174–83. doi:10.1159/000028398. PMID 10971203. S2CID 24471776.
- Bertilsson L (September 1995). "Geographical/interracial differences in polymorphic drug oxidation. Current state of knowledge of cytochromes P450 (CYP) 2D6 and 2C19". Clinical Pharmacokinetics. 29 (3): 192–209. doi:10.2165/00003088-199529030-00005. PMID 8521680. S2CID 111743.
- Desta Z, Zhao X, Shin JG, Flockhart DA (2002). "Clinical significance of the cytochrome P450 2C19 genetic polymorphism". Clinical Pharmacokinetics. 41 (12): 913–58. doi:10.2165/00003088-200241120-00002. PMID 12222994. S2CID 27616494.
- Ionova Y, Ashenhurst J, Zhan J, Nhan H, Kosinski C, Tamraz B, Chubb A (June 2020). "CYP2C19 allele frequencies in over 2.2 million direct-to-consumer genetics research participants and the potential implication for prescriptions in a large health system". Clinical and Translational Science. 13 (6): 1298–1306. doi:10.1111/cts.12830. PMC 7719394. PMID 32506666.
- Reference, Genetics Home. "CYP2C19 gene". Genetics Home Reference. Retrieved 6 March 2020.
- Forest, Tennant (2014). "American Association of Clinical Chemistry Annual Meeting 2014: Utility of Genetic Testing in Practical Pain Management". AutoGenomics.
- Li-Wan-Po A, Girard T, Farndon P, Cooley C, Lithgow J (March 2010). "Pharmacogenetics of CYP2C19: functional and clinical implications of a new variant CYP2C19*17". British Journal of Clinical Pharmacology. 69 (3): 222–30. doi:10.1111/j.1365-2125.2009.03578.x. PMC 2829691. PMID 20233192.
- Klotz U, Schwab M, Treiber G (July 2004). "CYP2C19 polymorphism and proton pump inhibitors". Basic & Clinical Pharmacology & Toxicology. 95 (1): 2–8. doi:10.1111/j.1600-0773.2004.pto950102.x. PMID 15245569.
- David Mrazek (2010). Psychiatric Pharmacogenomics. p. 62. ISBN 9780195367294.
- Bernini de Brito R, Ghedini PC (May 2020). "CYP2C19 polymorphisms and outcomes of Escitalopram treatment in Brazilians with major depression". Heliyon. 6 (5): e04015. doi:10.1016/j.heliyon.2020.e04015. PMC 7264488. PMID 32509985.
- Lee, C. R.; Thomas, C. D.; Beitelshees, A. L.; Tuteja, S.; Empey, P. E.; Lee, J. C.; Limdi, N. A.; Duarte, J. D.; Skaar, T. C.; Chen, Y.; Cook, K. J.; Coons, J. C.; Dillon, C.; Franchi, F.; Giri, J.; Gong, Y.; Kreutz, R. P.; McDonough, C. W.; Stevenson, J. M.; Weck, K. E.; Angiolillo, D. J.; Johnson, J. A.; Stouffer, G. A.; Cavallari, L. H.; IGNITE Network Pharmacogenetics Working Group (2020). "Impact of the CYP2C19*17 Allele on Outcomes in Patients Receiving Genotype-Guided Antiplatelet Therapy After Percutaneous Coronary Intervention". Clinical Pharmacology and Therapeutics. doi:10.1002/cpt.2039. PMID 32897581.
- Sibbing D, Koch W, Gebhard D, Schuster T, Braun S, Stegherr J, et al. (February 2010). "Cytochrome 2C19*17 allelic variant, platelet aggregation, bleeding events, and stent thrombosis in clopidogrel-treated patients with coronary stent placement". Circulation. 121 (4): 512–8. doi:10.1161/CIRCULATIONAHA.109.885194. PMID 20083681. S2CID 13408332.
- Li Y, Tang HL, Hu YF, Xie HG (February 2012). "The gain-of-function variant allele CYP2C19*17: a double-edged sword between thrombosis and bleeding in clopidogrel-treated patients". Journal of Thrombosis and Haemostasis. 10 (2): 199–206. doi:10.1111/j.1538-7836.2011.04570.x. PMID 22123356. S2CID 35503064.
- Rudberg, I.; Mohebi, B.; Hermann, M.; Refsum, H.; Molden, E. (2008). "Impact of the ultrarapid CYP2C19*17 allele on serum concentration of escitalopram in psychiatric patients". Clinical Pharmacology and Therapeutics. 83 (2): 322–7. doi:10.1038/sj.clpt.6100291. PMID 17625515. S2CID 7772078.
- Paré G, Mehta SR, Yusuf S, Anand SS, Connolly SJ, Hirsh J, et al. (October 2010). "Effects of CYP2C19 genotype on outcomes of clopidogrel treatment" (PDF). The New England Journal of Medicine. 363 (18): 1704–14. doi:10.1056/NEJMoa1008410. PMID 20979470.
- Center for Drug Evaluation and Research. "Drug Interactions & Labeling - Drug Development and Drug Interactions: Table of Substrates, Inhibitors and Inducers". FDA. Retrieved 1 June 2016.
- Flockhart, DA (2007). "Drug Interactions: Cytochrome P450 Drug Interaction Table". Indiana University School of Medicine. Retrieved 10 July 2011.
- Sjöqvist, Folke. "Fakta för förskrivare: Interaktion mellan läkemedel" [Facts for prescribers: Interaction between drugs]. FASS Vårdpersonal (in Swedish). Retrieved 10 July 2011.
- Zhu AZ, Zhou Q, Cox LS, Ahluwalia JS, Benowitz NL, Tyndale RF (November 2014). "Gene variants in CYP2C19 are associated with altered in vivo bupropion pharmacokinetics but not bupropion-assisted smoking cessation outcomes". Drug Metabolism and Disposition. 42 (11): 1971–7. doi:10.1124/dmd.114.060285. PMC 4201132. PMID 25187485.
- Miyazawa M, Shindo M, Shimada T (May 2002). "Metabolism of (+)- and (-)-limonenes to respective carveols and perillyl alcohols by CYP2C9 and CYP2C19 in human liver microsomes". Drug Metabolism and Disposition. 30 (5): 602–7. doi:10.1124/dmd.30.5.602. PMID 11950794.
- Zhang Y, Si D, Chen X, Lin N, Guo Y, Zhou H, Zhong D (July 2007). "Influence of CYP2C9 and CYP2C19 genetic polymorphisms on pharmacokinetics of gliclazide MR in Chinese subjects". British Journal of Clinical Pharmacology. 64 (1): 67–74. doi:10.1111/j.1365-2125.2007.02846.x. PMC 2000619. PMID 17298483.
- Xu H, Williams KM, Liauw WS, Murray M, Day RO, McLachlan AJ (April 2008). "Effects of St John's wort and CYP2C9 genotype on the pharmacokinetics and pharmacodynamics of gliclazide". British Journal of Pharmacology. 153 (7): 1579–86. doi:10.1038/sj.bjp.0707685. PMC 2437900. PMID 18204476.
- "Drug Development and Drug Interactions: Table of Substrates, Inhibitors and Inducers".
- Park JY, Kim KA, Kim SL (November 2003). "Chloramphenicol is a potent inhibitor of cytochrome P450 isoforms CYP2C19 and CYP3A4 in human liver microsomes". Antimicrobial Agents and Chemotherapy. 47 (11): 3464–9. doi:10.1128/AAC.47.11.3464-3469.2003. PMC 253795. PMID 14576103.
- Sager JE, Lutz JD, Foti RS, Davis C, Kunze KL, Isoherranen N (June 2014). "Fluoxetine- and norfluoxetine-mediated complex drug-drug interactions: in vitro to in vivo correlation of effects on CYP2D6, CYP2C19, and CYP3A4". Clinical Pharmacology and Therapeutics. 95 (6): 653–62. doi:10.1038/clpt.2014.50. PMC 4029899. PMID 24569517.
- Perucca E, Levy RH (2002). "Combination Therapy and Drug Interactions". In Levy RH, Mattson RH, Meldrum BS, Perucca E (eds.). Antiepileptic drugs (5th ed.). Hagerstwon, MD: Lippincott Williams & Wilkins. p. 100. ISBN 0-7817-2321-3. OCLC 848759609.
- Gjestad C, Westin AA, Skogvoll E, Spigset O (February 2015). "Effect of proton pump inhibitors on the serum concentrations of the selective serotonin reuptake inhibitors citalopram, escitalopram, and sertraline". Therapeutic Drug Monitoring. 37 (1): 90–7. doi:10.1097/FTD.0000000000000101. PMC 4297217. PMID 24887634.
- Wen X, Wang JS, Neuvonen PJ, Backman JT (January 2002). "Isoniazid is a mechanism-based inhibitor of cytochrome P450 1A2, 2A6, 2C19 and 3A4 isoforms in human liver microsomes". European Journal of Clinical Pharmacology. 57 (11): 799–804. doi:10.1007/s00228-001-0396-3. PMID 11868802. S2CID 19299097.
- Chen XP, Tan ZR, Huang SL, Huang Z, Ou-Yang DS, Zhou HH (March 2003). "Isozyme-specific induction of low-dose aspirin on cytochrome P450 in healthy subjects". Clinical Pharmacology and Therapeutics. 73 (3): 264–71. doi:10.1067/mcp.2003.14. PMID 12621391. S2CID 24772442.
Further reading
- Goldstein JA, de Morais SM (December 1994). "Biochemistry and molecular biology of the human CYP2C subfamily". Pharmacogenetics. 4 (6): 285–99. doi:10.1097/00008571-199412000-00001. PMID 7704034.
- Smith G, Stubbins MJ, Harries LW, Wolf CR (December 1998). "Molecular genetics of the human cytochrome P450 monooxygenase superfamily". Xenobiotica. 28 (12): 1129–65. doi:10.1080/004982598238868. PMID 9890157.
- Ding X, Kaminsky LS (2003). "Human extrahepatic cytochromes P450: function in xenobiotic metabolism and tissue-selective chemical toxicity in the respiratory and gastrointestinal tracts". Annual Review of Pharmacology and Toxicology. 43: 149–73. doi:10.1146/annurev.pharmtox.43.100901.140251. PMID 12171978.
- Meier UT, Meyer UA (December 1987). "Genetic polymorphism of human cytochrome P-450 (S)-mephenytoin 4-hydroxylase. Studies with human autoantibodies suggest a functionally altered cytochrome P-450 isozyme as cause of the genetic deficiency". Biochemistry. 26 (25): 8466–74. doi:10.1021/bi00399a065. PMID 3442670.
- De Morais SM, Wilkinson GR, Blaisdell J, Meyer UA, Nakamura K, Goldstein JA (October 1994). "Identification of a new genetic defect responsible for the polymorphism of (S)-mephenytoin metabolism in Japanese". Molecular Pharmacology. 46 (4): 594–8. PMID 7969038.
- Romkes M, Faletto MB, Blaisdell JA, Raucy JL, Goldstein JA (February 1993). "Cloning and expression of complementary DNAs for multiple members of the human cytochrome PH50IIC subfamily". Biochemistry. 32 (5): 1390. doi:10.1021/bi00056a025. PMID 8095407.
- Goldstein JA, Faletto MB, Romkes-Sparks M, Sullivan T, Kitareewan S, Raucy JL, Lasker JM, Ghanayem BI (February 1994). "Evidence that CYP2C19 is the major (S)-mephenytoin 4'-hydroxylase in humans". Biochemistry. 33 (7): 1743–52. doi:10.1021/bi00173a017. PMID 8110777.
- de Morais SM, Wilkinson GR, Blaisdell J, Nakamura K, Meyer UA, Goldstein JA (June 1994). "The major genetic defect responsible for the polymorphism of S-mephenytoin metabolism in humans". The Journal of Biological Chemistry. 269 (22): 15419–22. doi:10.1016/S0021-9258(17)40694-6. PMID 8195181.
- Karam WG, Goldstein JA, Lasker JM, Ghanayem BI (October 1996). "Human CYP2C19 is a major omeprazole 5-hydroxylase, as demonstrated with recombinant cytochrome P450 enzymes". Drug Metabolism and Disposition. 24 (10): 1081–7. PMID 8894508.
- Xiao ZS, Goldstein JA, Xie HG, Blaisdell J, Wang W, Jiang CH, Yan FX, He N, Huang SL, Xu ZH, Zhou HH (April 1997). "Differences in the incidence of the CYP2C19 polymorphism affecting the S-mephenytoin phenotype in Chinese Han and Bai populations and identification of a new rare CYP2C19 mutant allele". The Journal of Pharmacology and Experimental Therapeutics. 281 (1): 604–9. PMID 9103550.
- Guengerich FP, Johnson WW (December 1997). "Kinetics of ferric cytochrome P450 reduction by NADPH-cytochrome P450 reductase: rapid reduction in the absence of substrate and variations among cytochrome P450 systems". Biochemistry. 36 (48): 14741–50. doi:10.1021/bi9719399. PMID 9398194.
- Ferguson RJ, De Morais SM, Benhamou S, Bouchardy C, Blaisdell J, Ibeanu G, Wilkinson GR, Sarich TC, Wright JM, Dayer P, Goldstein JA (January 1998). "A new genetic defect in human CYP2C19: mutation of the initiation codon is responsible for poor metabolism of S-mephenytoin". The Journal of Pharmacology and Experimental Therapeutics. 284 (1): 356–61. PMID 9435198.
- Ibeanu GC, Goldstein JA, Meyer U, Benhamou S, Bouchardy C, Dayer P, Ghanayem BI, Blaisdell J (September 1998). "Identification of new human CYP2C19 alleles (CYP2C19*6 and CYP2C19*2B) in a Caucasian poor metabolizer of mephenytoin". The Journal of Pharmacology and Experimental Therapeutics. 286 (3): 1490–5. PMID 9732415.
- Ibeanu GC, Blaisdell J, Ghanayem BI, Beyeler C, Benhamou S, Bouchardy C, Wilkinson GR, Dayer P, Daly AK, Goldstein JA (April 1998). "An additional defective allele, CYP2C19*5, contributes to the S-mephenytoin poor metabolizer phenotype in Caucasians". Pharmacogenetics. 8 (2): 129–35. doi:10.1097/00008571-199804000-00006. PMID 10022751.
- Foster DJ, Somogyi AA, Bochner F (April 1999). "Methadone N-demethylation in human liver microsomes: lack of stereoselectivity and involvement of CYP3A4". British Journal of Clinical Pharmacology. 47 (4): 403–12. doi:10.1046/j.1365-2125.1999.00921.x. PMC 2014231. PMID 10233205.
- Ibeanu GC, Blaisdell J, Ferguson RJ, Ghanayem BI, Brosen K, Benhamou S, Bouchardy C, Wilkinson GR, Dayer P, Goldstein JA (August 1999). "A novel transversion in the intron 5 donor splice junction of CYP2C19 and a sequence polymorphism in exon 3 contribute to the poor metabolizer phenotype for the anticonvulsant drug S-mephenytoin". The Journal of Pharmacology and Experimental Therapeutics. 290 (2): 635–40. PMID 10411572.
External links
- PharmGKB: Annotated PGx Gene Information for CYP2C19
- Human CYP2C19 genome location and CYP2C19 gene details page in the UCSC Genome Browser.