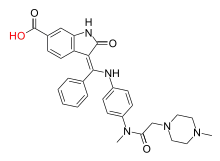
Nintedanib
Nintedanib, sold under the brand names Ofev and Vargatef, is an oral medication used for the treatment of idiopathic pulmonary fibrosis and along with other medications for some types of non-small-cell lung cancer.[2]
 Nintedanib | |
| Clinical data | |
|---|---|
| Trade names | Vargatef, Ofev |
| Other names | BIBF 1120 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a615009 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 4.7% |
| Protein binding | 97.8% |
| Metabolism | Esterases, glucuronidation |
| Elimination half-life | 10–15 hrs |
| Excretion | 93% via faeces |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| ECHA InfoCard | 100.237.441 |
| Chemical and physical data | |
| Formula | C31H33N5O4 |
| Molar mass | 539.636 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
In March 2020, it was approved for use in the United States to treat chronic fibrosing (scarring) interstitial lung diseases (ILD) with a progressive phenotype (trait).[3] It is the first treatment for this group of fibrosing lung diseases that worsen over time that was approved by the U.S. Food and Drug Administration (FDA).[3]
Common side effects include abdominal pain, vomiting, and diarrhea.[4] It is a small molecule tyrosine-kinase inhibitor, targeting vascular endothelial growth factor receptor, fibroblast growth factor receptor and platelet derived growth factor receptor.
Ofev was developed by Boehringer Ingelheim. It received U.S. Food and Drug Administration (FDA) approval for use for idiopathic pulmonary fibrosis in 2014 - one of only two drugs available for treating IPF - and numerous studies since have demonstrated its effectiveness in slowing the progressive, terminal lung disease.[5]
Medical uses
Idiopathic pulmonary fibrosis
Nintedanib is used for the treatment of idiopathic pulmonary fibrosis.[6] It has been shown to slow down decrease in forced vital capacity,[7][8] and it also improves people's quality of life.[9] Nintedanib does not improve survival in people with IPF.[10] It interferes with processes like fibroblast proliferation, differentiation and laying down extracellular matrix.[11] The National Institute for Health and Care Excellence (NICE) recommends nintedanib in cases of IPF where the FVC is 50-80% of predicted. NICE recommends discontinuation of therapy if a person's FVC decreases by 10% or more in a 12-month period, indicating disease progression despite treatment.[12]
Lung cancer
It is also used in combination with docetaxel as a second-line treatment for adult patients with locally advanced, metastatic, or locally recurring non-small cell lung cancer of adenocarcinoma histology.[13] It is unclear how this combination compares to other second line agents as the comparisons have not been done as of 2014.[13]
Contraindications
Nintedanib is contraindicated in patients with known hypersensitivity to nintedanib, peanut or soya.[14] Nintedanib has not been tested in patients with moderate to severe impairment of liver function. Given that the drug is metabolised in the liver, it may not be safe in such patients.[15] Nintedanib can be used in geriatric population without any dose modifications. It has not been studied in paediatric populations and hence cannot be given in patients below 18 years of age. It is also contraindicated in pregnancy[14]
Adverse effects
Common side effects noted with nintedanib include anorexia, nausea, vomiting, diarrhea, abdominal pain, gastrointestinal perforation, weight loss, arterial thromboembolism (including myocardial infarction), bleeding, hypothyroidism, elevated liver enzymes, and headache. Gastrointestinal side effects are decreased when nintedanib is co-administered with food.[12]
Side effects observed with nintedanib were worse with a higher dose. For this reason, subsequent trials have used an equally clinically effective lower dose.[16][17][18][19][20][21][22][23][24]
Pharmacology
Mechanism of action
Nintedanib competitively inhibits both nonreceptor tyrosine kinases (nRTKs) and receptor tyrosine kinases (RTKs). NRTK targets of nintedanib include Lck, Lyn, and Src. RTK targets of nintedanib include platelet-derived growth factor receptor (PDGFR) α and β; fibroblast growth factor receptor (FGFR) 1, 2, and 3; vascular endothelial growth factor receptor (VEGFR) 1, 2, and 3; and FLT3. Its use in IPF is predicated on its inhibition of PDGFR, FGFR, and VEGFR, which increase fibroblast proliferation, migration, and transformation.[12]
Pharmacokinetics
Only a small percentage of orally taken nintedanib is absorbed in the gut, partially due to transport proteins (such as P-glycoprotein) moving the substance back into the lumen. Combined with a high first-pass effect, this results in an oral bioavailability of about 4.7% with a 100 mg tablet.[25][14][15] The drug reaches peak plasma levels in 2 to 4 hours after oral intake in the form of a soft gelatin capsule.[14]
Nintedanib is mainly inactivated by esterases that cleave the methyl ester, resulting in the free carboxylic acid form, which is then glucuronidated by uridinediphosphate-glucuronosyltransferases and excreted mostly via the bile and faeces. No relevant cytochrome P450 mediated metabolism has been observed.[15]
Interactions
Nintedanib is a substrate of the transporter P-glycoprotein which moves the absorbed substance back into the gut's lumen. The P-glycoprotein inhibitor ketoconazole is known to increase blood plasma levels of nintedanib by a factor of 1.8; other inhibitors such as erythromycin or ciclosporin are expected to have a similar effect. On the other hand, the P-glycoprotein inducer rifampicin cuts nintedanib plasma levels in half; other inducers such as carbamazepine, phenytoin or St. John's Wort probably lower plasma levels as well.[15]
Chemistry
The drug is used in form of its salt with ethanesulfonic acid. This salt, nintedanib esilate, is a yellow, crystalline solid that melts at 244 °C (471 °F) to 251 °C (484 °F). It has poor solubility in water, and somewhat better solubility in dimethyl sulfoxide at 25 g/l.[26]
History
Idiopathic pulmonary fibrosis
Nintedanib was approved for idiopathic pulmonary fibrosis on 15 October 2014, by the United States Food and Drug Administration (FDA),[27] and received a positive opinion from the European Medicines Agency on 20 November 2014, being approved in the European Union in January 2015.[28][29] It is also approved in Canada, Japan, Switzerland, and other countries.[30]
Two replicate randomized clinical trials evaluated the efficacy and safety of nintedanib for the treatment of idiopathic pulmonary fibrosis.[31] The primary endpoint of the study was the effect on lung function, measured by forced vital capacity. In total, 1066 patients were treated with either 150 mg nintedanib or placebo and evaluated after 52 weeks. At the end of the observation period, nintedanib reduced the decline of forced vital capacity.[31] In the study, diarrhoea was the most common adverse event and was higher in the nintedanib group compared to the placebo group.[31]
Nintedanib was granted orphan drug designation in the US by the FDA for the treatment of idiopathic pulmonary fibrosis in June 2011 until 15 October 2021.[32]
Lung cancer
Nintedanib was approved for combination therapy of non-small-cell lung cancer in the European Union in 2014,[15][33] and is approved for this indication in other parts of the world.[30]
Nintedanib was granted orphan drug designation in the US by the FDA for the treatment of systemic sclerosis (including the associated interstitial lung disease) in July 2016 until 6 September 2019.[34]
Other interstitial lung diseases
The drug was granted priority review designation by the FDA before being approved in the US on 6 September 2019, to slow the rate of decline in pulmonary function in patients with systemic sclerosis associated interstitial lung disease (SSc-ILD).[35][36] It is the first FDA-approved treatment for this rare lung condition.[35] The effectiveness of nintedanib to treat SSc-ILD was studied in a randomized, double-blind, placebo-controlled trial of 576 subjects ages 20–79 with the disease.[35] Subjects received treatment for 52 weeks, with some subjects treated up to 100 weeks.[35] The primary test for efficacy measured the forced vital capacity, or FVC, which is a measure of lung function, defined as the amount of air that can be forcibly exhaled from the lungs after taking the deepest breath possible.[35] Those who took nintedanib had less lung function decline compared to those on placebo.[35] The overall safety profile observed in the nintedanib treatment group was consistent with the known safety profile of the therapy.[35] The most frequent serious adverse event reported in subjects treated with nintedanib was pneumonia (2.8% nintedanib vs. 0.3% placebo).[35] Adverse reactions leading to permanent dose reductions were reported in 34% of nintedanib-treated subjects compared to 4% of placebo-treated subjects.[35] Diarrhea was the most frequent adverse reaction that led to permanent dose reduction in subjects treated with nintedanib.[35]
The safety and effectiveness of nintedanib to treat chronic fibrosing interstitial lung diseases with a progressive phenotype in adults was evaluated in a randomized, double-blind, placebo-controlled study of 663 adults.[3] The mean age of subjects was 66 years and more subjects were male (54%) than female.[3] The primary test for effectiveness was the forced vital capacity, which is a measure of lung function.[3] It is defined as the amount of air that can be forcibly exhaled from the lungs after taking the deepest breath possible.[3] In the 52-week period, subjects received either 150 milligrams of nintedanib twice a day or a placebo.[3] After 52 weeks, people who received nintedanib had less lung function decline compared to those on the placebo.[3]
The US Food and Drug Administration (FDA) granted nintedanib priority review designation and breakthrough therapy designation.[3] The FDA granted the approval of Ofev to Boehringer Ingelheim Pharmaceuticals, Inc.[3]
Society and culture
Boehringer is using the brand name Ofev for marketing nintedanib for idiopathic pulmonary fibrosis and Vargatef for marketing the medication for lung cancer.[37]
Research
Nintedanib is being tested in several phase I to III clinical trials for cancer. Angiogenesis inhibitors such as nintedanib may be effective in a range of solid tumour types including lung, ovarian, metastatic bowel, liver and brain cancer.
Current phase II trials are investigating the effect of nintedanib in patients with bladder cancer, metastatic bowel cancer, liver cancer and the brain tumour glioblastoma multiforme.[38]
Phase III trials are investigating the use of nintedanib in combination with carboplatin and paclitaxel as a first line treatment for patients with ovarian cancer.[39]
References
- "Nintedanib (Ofev) Use During Pregnancy". Drugs.com. 16 September 2019. Retrieved 9 March 2020.
- "Vargatef EPAR". European Medicines Agency (EMA). 20 January 2020. Retrieved 9 March 2020.
- "FDA Approves First Treatment for Group of Progressive Interstitial Lung Diseases". U.S. Food and Drug Administration (FDA) (Press release). 9 March 2020. Retrieved 9 March 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "Nintedanib Side Effects". Retrieved 24 October 2015.
- "Nintedanib".
- "Nintedanib". drugs.com. Retrieved 12 February 2015.
- Ahluwalia N, Shea BS, Tager AM (October 2014). "New therapeutic targets in idiopathic pulmonary fibrosis. Aiming to rein in runaway wound-healing responses". American Journal of Respiratory and Critical Care Medicine. 190 (8): 867–78. doi:10.1164/rccm.201403-0509pp. PMC 4299574. PMID 25090037.
- Mazzei ME, Richeldi L, Collard HR (June 2015). "Nintedanib in the treatment of idiopathic pulmonary fibrosis". Therapeutic Advances in Respiratory Disease. 9 (3): 121–9. doi:10.1177/1753465815579365. PMID 25862013.
- Dimitroulis IA (September 2014). "Nintedanib: a novel therapeutic approach for idiopathic pulmonary fibrosis". Respiratory Care. 59 (9): 1450–5. doi:10.4187/respcare.03023. PMID 24782550.
- Brunton L, Knollman B, Hilal-Dandan R (26 October 2017). Goodman and Gilman's The Pharmacological Basis of Therapeutics, 13th Edition. McGraw Hill Professional. ISBN 9781259584749.
- Wollin, Lutz; Wex, Eva; Pautsch, Alexander; Schnapp, Gisela; Hostettler, Katrin E.; Stowasser, Susanne; Kolb, Martin (5 March 2015). "Mode of action of nintedanib in the treatment of idiopathic pulmonary fibrosis". European Respiratory Journal. 45 (5): 1434–1445. doi:10.1183/09031936.00174914. ISSN 0903-1936. PMC 4416110. PMID 25745043.
- "Nintedanib for treating idiopathic pulmonary fibrosis" (PDF). National Institute for Health and Care Excellence (NICE). 27 January 2016. TA379. Retrieved 7 August 2019. Lay summary.
- Popat S, Mellemgaard A, Fahrbach K, Martin A, Rizzo M, Kaiser R, et al. (5 December 2014). "Nintedanib plus docetaxel as second-line therapy in patients with non-small-cell lung cancer: a network meta-analysis". Future Oncology. 11 (3): 409–20. doi:10.2217/fon.14.290. PMID 25478720.
- "Product monograph" (PDF). 10 October 2018. Retrieved 16 October 2018.
- Haberfeld H (ed.). Austria-Codex (in German) (2014/2015 ed.). Vienna: Österreichischer Apothekerverlag.
- Hilberg F, Tontsch-Grunt U, Colbatzky F, Heckel A, Lotz R, van Meel JC, Roth GJ (2004). "BIBF1120 a novel, small molecule triple angiokinase inhibitor: profiling as a clinical candidate for cancer therapy". European Journal of Cancer Supplements. 2 (50): 50. doi:10.1016/S1359-6349(04)80166-6.
- Hilberg F, Roth GJ, Krssak M, Kautschitsch S, Sommergruber W, Tontsch-Grunt U, et al. (June 2008). "BIBF 1120: triple angiokinase inhibitor with sustained receptor blockade and good antitumor efficacy". Cancer Research. 68 (12): 4774–82. doi:10.1158/0008-5472.CAN-07-6307. PMID 18559524.
- Reck M, Kaiser R, Eschbach C, Stefanic M, Love J, Gatzemeier U, et al. (June 2011). "A phase II double-blind study to investigate efficacy and safety of two doses of the triple angiokinase inhibitor BIBF 1120 in patients with relapsed advanced non-small-cell lung cancer". Annals of Oncology. 22 (6): 1374–81. doi:10.1093/annonc/mdq618. PMID 21212157.
- Okamoto I, Kaneda H, Satoh T, Okamoto W, Miyazaki M, Morinaga R, et al. (October 2010). "Phase I safety, pharmacokinetic, and biomarker study of BIBF 1120, an oral triple tyrosine kinase inhibitor in patients with advanced solid tumors". Molecular Cancer Therapeutics. 9 (10): 2825–33. doi:10.1158/1535-7163.MCT-10-0379. PMID 20688946.
- Mross K, Stefanic M, Gmehling D, Frost A, Baas F, Unger C, et al. (January 2010). "Phase I study of the angiogenesis inhibitor BIBF 1120 in patients with advanced solid tumors". Clinical Cancer Research. 16 (1): 311–9. doi:10.1158/1078-0432.CCR-09-0694. PMID 20028771.
- Ledermann JA (2009). "A randomised phase II placebo-controlled trial using maintenance therapy to evaluate the vascular targeting agent BIBF 1120 following treatment of relapsed ovarian cancer (OC)". Journal of Clinical Oncology. 27 (15s): (suppl, abstr 5501). doi:10.1200/jco.2009.27.15_suppl.5501.
- Kropff M, Kienast J, Bisping G, Berdel WE, Gaschler-Markefski B, Stopfer P, et al. (October 2009). "An open-label dose-escalation study of BIBF 1120 in patients with relapsed or refractory multiple myeloma". Anticancer Research. 29 (10): 4233–8. PMID 19846979.
- Ellis PM, Kaiser R, Zhao Y, Stopfer P, Gyorffy S, Hanna N (May 2010). "Phase I open-label study of continuous treatment with BIBF 1120, a triple angiokinase inhibitor, and pemetrexed in pretreated non-small cell lung cancer patients". Clinical Cancer Research. 16 (10): 2881–9. doi:10.1158/1078-0432.CCR-09-2944. PMID 20460487.
- du Bois A, Huober J, Stopfer P, Pfisterer J, Wimberger P, Loibl S, et al. (February 2010). "A phase I open-label dose-escalation study of oral BIBF 1120 combined with standard paclitaxel and carboplatin in patients with advanced gynecological malignancies". Annals of Oncology. 21 (2): 370–5. doi:10.1093/annonc/mdp506. PMID 19889612.
- "PRODUCT MONOGRAPH" (PDF). www.boehringer-ingelheim.ca. 10 August 2018. Retrieved 12 June 2019.
- Sicherheitsdatenblatt [Safety data sheet] Nintedanibesilat (in German)
- "FDA Approves Ofev". drugs.com. Retrieved 12 February 2015.
- "Ofev EPAR". European Medicines Agency (EMA). 20 January 2020. Retrieved 9 March 2020.
- "OFEV (nintedanib*) approved in the EU for the treatment of IPF". Boehringer Ingelheim Press Release Archive. 19 January 2015. Retrieved 13 May 2015.
- "LexiComp". Wolters Kluwer Clinical Drug Information.
- Richeldi L, du Bois RM, Raghu G, Azuma A, Brown K, Costabel U, Cottin V, Flaherty KR, Hansell DM, Inoue Y, Kim DS, Kolb M, Nicholson AG, Noble PW, Selman M, Taniguchi H, Brun M, Le Maulf F, Girard M, Stowasser S, Schlenker-Herceg R, Disse B, Collard HR, INPULSIS Trial Investigators (May 2014). "Efficacy and Safety of Nintedanib in Idiopathic Pulmonary Fibrosis". N Engl J Med. 370 (22): 2071–82. doi:10.1056/NEJMoa1402584. PMID 24836310.
- "Nintedanib Orphan Drug Designation and Approval". U.S. Food and Drug Administration (FDA). Retrieved 9 March 2020.
- "Vargatef (nintedanib*) approved in the EU for lung cancer patients with advanced adenocarcinoma after first-line chemotherapy". Boehringer Ingelheim Press Release Archive. 27 November 2014. Archived from the original on 12 May 2015. Retrieved 13 May 2015.
- "Nintedanib Orphan Drug Designation and Approval". U.S. Food and Drug Administration (FDA). Retrieved 9 March 2020.
- "FDA approves first treatment for patients with rare type of lung disease" (Press release). 6 September 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - https://www.boehringer-ingelheim.com/press-release/fda-approves-nintedanib-ssc-ild
- "Boehringer's Ofev approved by FDA for rare lung disease". 17 October 2014. Retrieved 24 October 2015.
- ClinicalTrials.gov: BIBF 1120
- Clinical trial number NCT01015118 for "LUME-Ovar 1: Nintedanib (BIBF 1120) or Placebo in Combination With Paclitaxel and Carboplatin in First Line Treatment of Ovarian Cancer" at ClinicalTrials.gov
External links
- "Nintedanib". Drug Information Portal. U.S. National Library of Medicine.
