Diving disorders
Diving disorders, or diving related medical conditions, are conditions associated with underwater diving, and include both conditions unique to underwater diving, and those that also occur during other activities. This second group further divides into conditions caused by exposure to ambient pressures significantly different from surface atmospheric pressure, and a range of conditions caused by general environment and equipment associated with diving activities.
Disorders particularly associated with diving include those caused by variations in ambient pressure, such as barotraumas of descent and ascent, decompression sickness and those caused by exposure to elevated ambient pressure, such as some types of gas toxicity. There are also non-dysbaric disorders associated with diving, which include the effects of the aquatic environment, such as drowning, which also are common to other water users, and disorders caused by the equipment or associated factors, such as carbon dioxide and carbon monoxide poisoning. General environmental conditions can lead to another group of disorders, which include hypothermia and motion sickness, injuries by marine and aquatic organisms, contaminated waters, man-made hazards, and ergonomic problems with equipment. Finally there are pre-existing medical and psychological conditions which increase the risk of being affected by a diving disorder, which may be aggravated by adverse side effects of medications and other drug use.
Treatment depends on the specific disorder, but often includes oxygen therapy, which is standard first aid for most diving accidents, and is hardly ever contra-indicated for a person medically fit to dive, and hyperbaric therapy is the definitive treatment for decompression sickness. Screening for medical fitness to dive can reduce some of the risk for some of the disorders.
Effects of variation in ambient pressure

Many diving accidents or illnesses are related to the effect of pressure on gases in the body;
Barotrauma
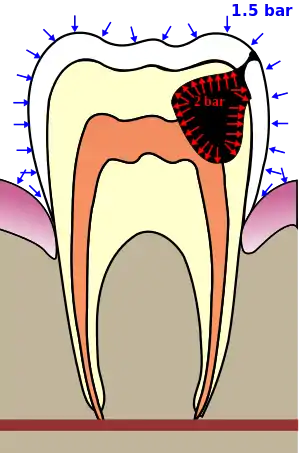
Barotrauma is physical injury to body tissues caused by a difference in pressure between a gas space inside or in contact with the body, and the surroundings.[1][2]
Barotrauma occurs when the difference in pressure between the surroundings and the gas space makes the gas expand in volume, distorting adjacent tissues enough to rupture cells or damage tissue by deformation. A special case, where pressure in tissue is reduced to the level that causes dissolved gas to come out of solution as bubbles, is called decompression sickness, the bends, or caisson disease.
Several organs are susceptible to barotrauma, however the cause is well understood and procedures for avoidance are clear. Nevertheless, barotrauma occurs and can be life-threatening, and procedures for first aid and further treatment are an important part of diving medicine.
- Barotraumas of descent (squeezes)
- Ear squeeze (also alternobaric vertigo)
- Sinus squeeze (aerosinusitis)
- Tooth squeeze (dental barotrauma, barodontalgia)
- Mask squeeze
- Helmet squeeze
- Suit squeeze
- Barotraumas of ascent (overexpansion injuries)
- Lung overexpansion injury (pulmonary barotrauma) – rupture of lung tissue allowing air to enter tissues, blood vessels, or spaces between or surrounding organs:
- Pneumothorax: Free air in the pleural cavity, leading to collapsed lung.
- Interstitial emphysema: Gas trapped in the spaces between tissues.
- Mediastinal emphysema: Gas trapped around the heart.
- Subcutaneous emphysema: Free gas under the skin.
- Arterial gas embolism: Air or other breathing gas in the blood stream, causing blockage of small blood vessels.
- Intestinal gas overexpansion
- Middle ear overpressure (reversed ear) (also alternobaric vertigo)
- Sinus overpressure (aerosinusitis)
- Tooth overpressure (dental barotrauma, barodontalgia)
- Lung overexpansion injury (pulmonary barotrauma) – rupture of lung tissue allowing air to enter tissues, blood vessels, or spaces between or surrounding organs:
Compression arthralgia
Decompression sickness
Dysbaric osteonecrosis
High pressure nervous syndrome
Nitrogen narcosis
Oxygen toxicity
Oxygen toxicity is a condition resulting from the harmful effects of breathing molecular oxygen (O
2) partial pressures significantly greater than found in atmospheric air at sea level. Severe cases can result in cell damage and death, with effects most often seen in the central nervous system, lungs and eyes.
Divers are exposed to raised partial pressures of oxygen in normal diving activities, where the partial pressure of oxygen in the breating gas is increased in proportion to the ambient pressure at depth, and by using gas mixtures in which oxygen is substituted for inert gases to reduce decompression obligations, to accelerate decompression, or reduce the risk of decompression sickness.
They are also exposed to raised partial pressures of oxygen if given oxygen as first aid, which is a standard protocol for most acute diving related disorders, and when undergoing hyperbaric oxygen therapy in the case of decompression sickness or arterial gas embolism.Non-dysbaric disorders associated with diving
Drowning
"Drowning is the process of experiencing respiratory impairment from submersion/immersion in liquid".[7]
Near drowning is the survival of a drowning event involving unconsciousness or water inhalation and can lead to serious secondary complications, including death, after the event.[8][9] Drowning is usually the culmination of a deteriorating sequence of events in a diving accident,and is seldom a satisfactory explanation for a fatatlity, as it fails to explain the underlying causes and complications that led to the final consequence.[10] Generally, a diver is well prepared for the environment, and well trained and equipped to deal with it. A diver should not drown merely as a result of being in the water.Salt water aspiration syndrome
Hypoxia
Hypoxia is a pathological condition in which the body as a whole or a region of the body is deprived of adequate oxygen supply. Variations in arterial oxygen concentrations can be part of the normal physiology, for example, during strenuous physical exercise. A mismatch between oxygen supply and its demand at the cellular level may result in a hypoxic condition.
Generalized hypoxia occurs when breathing mixtures of gases with a low oxygen content, e.g. while diving underwater especially when using closed-circuit rebreather systems that control the amount of oxygen in the supplied air, or when breathing gas mixtures blended to prevent oxygen toxicity at depths below about 60 m near or at the surface. This condition may lead to a loss if consciousness underwater and consequent death either directly by cerebral hypoxia, or indirectly by drowning.
Latent hypoxia may occur when a breathhold diver surfaces. This is also known as deep water blackout. The consequence is likely to be drowning.
Tissue hypoxia occurs when arterial gas emboli due to either lung overexpansion injury or decompression sickness block systemic capillaries and shut off the supply of oxygenated blood to the tissues downstream. If untreated, this leads to tissue damage or death, with consequences that depend on the site and extent of the injury.Swimming induced pulmonary edema
Swimming induced pulmonary edema occurs when fluids from the blood leak abnormally from the small vessels of the lung (pulmonary capillaries) into the airspaces (alveoli).[13]
SIPE usually occurs during heavy exertion in conditions of water immersion, such as swimming and diving. It has been reported in scuba divers,[14][15] apnea (breath hold) free-diving competitors,[16][17] combat swimmers,[18][19] and triathletes.[13] The causes are incompletely understood at the present time.[13][20][21]Immersion diuresis
Immersion diuresis is a type of diuresis caused by immersion of the body in water (or equivalent liquid). It is mainly caused by lower temperature and by pressure.
The temperature effect is caused by vasoconstriction of the cutaneous blood vessels within the body to conserve heat.[22][23][24] The body detects an increase in the blood pressure and inhibits the release of vasopressin, causing an increase in the production of urine.
The pressure effect is caused by the hydrostatic pressure of the water directly increasing blood pressure. Its significance is indicated by the fact that the temperature of the water doesn't substantially affect the rate of diuresis.[25] Partial immersion of only the limbs does not cause increased urination.
Diuresis is significant in diving medicine as the consequent mild dehydration may be a contributing factor in the onset of decompression sickness.Hypercapnia
Hypercapnia is a condition where there is too much carbon dioxide (CO2) in the blood.
Divers may develop this condition for several possible reasons:
- Increased work of breathing due to increased density of the breathing das with depth.[26][27][28][29]
- Inadequate ventilatory response to exertion.[26][27][28][29]
- Dead space of the breathing apparatus.[29]
- Higher inspired CO2 due to failure of the carbon dioxide scrubber in the diver's rebreather to remove sufficient carbon dioxide from the loop.
- Over-exertion, producing excess carbon dioxide due to elevated metabolic activity.
- Deliberate hypoventilation, known as "skip breathing".
- Shallow breathing, due to stress or other reasons.
- Contamination of the breathing gas supply.
Carbon monoxide poisoning
Carbon monoxide poisoning occurs by inhalation of carbon monoxide (CO). Carbon monoxide is a toxic gas, but, being colorless, odorless, tasteless, and initially non-irritating, it is very difficult for people to detect. Carbon monoxide is a product of incomplete combustion of organic matter due to insufficient oxygen supply to enable complete oxidation to carbon dioxide (CO2). Breathing gas for diving may be contaminated either by intake of contaminated atmospheric air, usually from internal combustion exhaust gases, or, more rarely, by carbon monoxide produced in the compressor by partial combustion of lubricants.[32]
The effects of carbon monoxide in breathing gas are increased in proportion to the depth, as the partial pressure of the contaminant is increased in proportion to the depth for a given gas fraction. The permitted levels of carbon monoxide in breathing gas for diving is lower than for at atmospheric pressure due to the concentratng effect of raised ambient pressure.Lipid pneumonia
Environmental hazards
Hazards in the underwater environment that can affect divers include marine life, marine infections, polluted water, ocean currents, waves and surges and man-made hazards such as boats, fishing lines and underwater construction. Diving medical personnel need to be able to recognize and treat accidents from large and small predators and poisonous creatures, appropriately diagnose and treat marine infections and illnesses from pollution as well as diverse maladies such as sea sickness, traveler's diarrhea and malaria.
Hypothermia
Hypothermia is a condition in which core temperature drops below the required temperature for normal metabolism and body functions (which is defined as 35.0 °C (95.0 °F)). Body temperature is usually maintained near a constant level of 36.5–37.5 °C (97.7–99.5 °F) through biological homeostasis or thermoregulation. If exposed to cold and the internal mechanisms are unable to replenish the heat that is being lost, a drop in core temperature occurs. As body temperature decreases, characteristic symptoms occur such as shivering and mental confusion.
Hypothermia usually occurs from exposure to low temperatures, but any condition that decreases heat production, increases heat loss, or impairs thermoregulation may contribute.[34] Heat is lost more quickly in water[35] than on land, and also more quickly in proportion to wind speed. Water temperatures that would be quite reasonable as outdoor air temperatures can lead to hypothermia. Divers are often exposed to low water temperatures and wind chill, which may be aggravated by evaporative cooling of wet dive suits, and mild hypothermia is not uncommon in both recreational and professional divers, while moderate to severe hypothermia remains a significant risk.Non-freezing cold injuries
Frostbite
Hyperthermia
Seasickness
Seasickness is a form of motion sickness, a condition in which a disagreement exists between visually perceived movement and the vestibular system's sense of movement[37] characterized by a feeling of nausea and, in extreme cases, vertigo, experienced after spending time on a craft on water,[38] floating at the surface of a rough sea, and in strong surge near the bottom.
Seasickness can significantly reduce the ability of a diver to effectively complete a task or manage a contingency, and may predispose the diver to hypothermia and decompression sickness.Cramps
Envenomation
Bites
Blunt trauma
Contamination from polluted waters
In most places, contamination comes from a variety of sources (non-point source pollution). In a few it is primarily pollution from a single industrial source. The more immediate threat is from locations where high concentrations of toxic or pathogenic pollutants are present, but lower concentrations of less immediately harmful contaminants can have a longer term influence on the diver's health. Three major categories of contamination can cause health and safety problems for divers. These are biological, chemical and radioactive materials.[39]
The risks from hazardous materials are generally proportional to dosage - exposure time and concentration, and the effects of the material on the body. This is particularly the case with chemical and radiological contaminants. There may be a threshold limit value which will not usually produce ill effects over long term exposure. Others may have a cumulative effect.[39]
The United Nations identification numbers for hazardous materials classifies hazardous materials under 9 categories:[39]
- Explosives
- Gases, which may be compressed, liquified or dissolved under pressure
- Flammable liquids
- Flammable solids
- Oxidising agents
- Poisonous and infectious substances
- Radioactive substances
- Corrosive substances
- Miscellaneous hazardous substances
A contaminant may be classed under one or more of these categories.
Poisonous substances are also classified in 9 categories:[39]
- Irritants
- Simple asphyxiants
- Blood asphyxiants
- Tissue asphyxiants
- Respiratory paralysers
- Liver and kidney toxins
- Substances that affect the muscles (myotoxins)
- Substances that affect bone marrow
- Substances tha interfere with nerve function (neurotoxins)
Trauma due to the natural physical environment
Injuries caused by man-made hazards
Disorders caused by the diving equipment
A variety of disorders may be caused by ergonomic problems due to poorly fitting equipment.
- Temporomandibular joint dysfunction is pain or tenderness in the jaw, headache or facial ache caused by gripping the regulator mouthpiece between the teeth of the upper and lower jaws. This action is required to retain the mouthpiece in place for the duration of the dive, and may strain the masticatory muscles or the temporomandibular joint, which is where the lower jawbone (mandible) hinges on the skull at the temporal bone. This problem van be aggravated by cold water, stress, and strong water movement, and can be reduced by use of custom mouthpieces with longer and more rigid bite grip surfaces, which allow better support of the second stage with less effort.[40]
- Leg and foot cramps may be caused by unaccustomed exercise, cold, or ill-fitting fins.
- Lower back pain may be caused by a heavy weightbelt hanging from the small of the back, counteracting the buoyancy of the diving suit which is distributed over the full length of the diver. This effect can be reduced by use of integrated weight systems which support the weights over the length of the back on the diving harness backplate.
- Restricted circulation to the hands may be caused by excessively tight dry suit cuff seals.
Treatment

Treatment of diving disorders depends on the specific disorder or combination of disorders, but two treatments are commonly associated with first aid and definitive treatment where diving is involved. These are first aid oxygen administration at high concentration, which is seldom contraindicated, and generally recommended as a default option in diving accidents where there is any significant probability of hypoxia, and hyperbaric oxygen therapy (HBO), which is the definitive treatment for most incidences of decompression illness. Hyperbaric treatment on other breathing gases is also used for treatment of decompression sickness if HBO is inadequate.
Oxygen therapy
The administration of oxygen as a medical intervention is common in diving medicine, both for first aid and for longer-term treatment.
Hyperbaric therapy
Recompression treatment in a hyperbaric chamber was initially used as a life-saving tool to treat decompression sickness in caisson workers and divers who stayed too long at depth and developed decompression sickness. Now, it is a highly specialized treatment modality that has been found to be effective in the treatment of many conditions where the administration of oxygen under pressure[41] has been found to be beneficial. Studies have shown it to be quite effective in some 13 indications approved by the Undersea and Hyperbaric Medical Society.[42]
Hyperbaric oxygen treatment is generally preferred when effective, as it is usually a more efficient and lower risk method of reducing symptoms of decompression illness, However, in some cases recompression to pressures where oxygen toxicity is unacceptable may be required to eliminate the bubbles in the tissues that cause the symptoms.
Fitness to dive

All divers should be free of conditions and illnesses that would negatively impact their safety and well-being underwater. The diving medical physician should be able to identify, treat and advise divers about illnesses and conditions that would cause them to be at increased risk for a diving accident.
Some reasons why a person should not be allowed to dive are as follows:
- Disorders that lead to altered consciousness: conditions that produce reduced awareness or sedation from medication, drugs, marijuana or alcohol; fainting, heart problems and seizure activity.
- Disorders that substantially increase the risk of barotrauma injury conditions or diseases that are associated with air trapping in closed spaces, such as sinuses, middle ear, lungs and gastrointestinal tract. Severe asthma is an example.
- Disorders that may lead to erratic and irresponsible behavior: included here would be immaturity, psychiatric disorders, diving while under the influence of medications, drugs and alcohol or any medical disorder that results in cognitive defects.
Conditions that may increase risk of diving disorders:
- Patent foramen ovale
- Diabetes mellitus — No serious problems should be expected during dives due to hypoglycaemia in divers with well-controlled diabetes. Long-term complications of diabetes should be considered and may be a contrindication.[43]
- Asthma
Conditions considered temporary reasons to suspend diving activities:
References
- US Navy Diving Manual, 6th revision. United States: US Naval Sea Systems Command. 2006. Retrieved 26 May 2008.
- Bennett, Peter B; Rostain, Jean Claude (2003). "The High Pressure Nervous Syndrome". In Brubakk, Alf O; Neuman, Tom S (eds.). Bennett and Elliott's physiology and medicine of diving (5th Rev ed.). United States: Saunders. pp. 323–57. ISBN 978-0-7020-2571-6.
- Campbell, Ernest (10 June 2010). "Compression arthralgia". Scubadoc's Diving Medicine Online. Retrieved 29 November 2013.
- Vann, Richard D, ed. (1989). "The Physiological Basis of Decompression". 38th Undersea and Hyperbaric Medical Society Workshop. 75(Phys)6–1–89: 437. Retrieved 15 May 2010.
- Brubakk, Alf O; Neuman. Tom S (2003). Bennett and Elliott's physiology and medicine of diving, 5th Rev ed. United States: Saunders Ltd. p. 800. ISBN 978-0-7020-2571-6.
- British Medical Research Council Decompression Sickness Central Registry and Radiological Panel (1981). "Aseptic bone necrosis in commercial divers. A report from the Decompression Sickness Central Registry and Radiological Panel". Lancet. 2 (8243): 384–8. doi:10.1016/s0140-6736(81)90831-x. PMID 6115158.
- E.F. van Beeck; C.M. Branche; D. Szpilman; J.H. Modell; J.J.L.M. Bierens (2005), A new definition of drowning: towards documentation and prevention of a global public health problem, 83, Bulletin of the World Health Organization (published 11 November 2005), pp. 801–880, retrieved 19 July 2012
- Lunetta, P.; Modell, J.H. (2005). Tsokos, M. (ed.). Macropathological, Microscopical, and Laboratory Findings in Drowning Victims. Forensic Pathology Reviews. 3. Totowa, NJ: Humana Pres Inc. pp. 4–77.
- Dueker CW, Brown SD, eds. (1999). "Near Drowning Workshop. 47th Undersea and Hyperbaric Medical Society Workshop". UHMS Publication Number WA292. Undersea and Hyperbaric Medical Society: 63. Retrieved 26 April 2009.
- Edmonds, C.; McKenzie, B.; Thomas, R.; Pennefather, J. (2013). Diving Medicine for Scuba Divers (free internet edition, 5th ed.). www.divingmedicine.info.
- Edmonds C (September 1970). "A salt water aspiration syndrome". Mil Med. 135 (9): 779–85. doi:10.1093/milmed/135.9.779. PMID 4991232.
- Edmonds C (1998). "Drowning syndromes: the mechanism". South Pacific Underwater Medicine Society Journal. 28 (1). ISSN 0813-1988. OCLC 16986801. Retrieved 4 July 2008.
- Miller III, Charles C.; Calder-Becker, Katherine; Modave, Francois (2010). "Swimming-induced pulmonary edema in triathletes". The American Journal of Emergency Medicine. 28 (8): 941–6. doi:10.1016/j.ajem.2009.08.004. PMID 20887912.
- Pons, M; Blickenstorfer, D; Oechslin, E; Hold, G; Greminger, P; Franzeck, UK; Russi, EW (1995). "Pulmonary oedema in healthy persons during scuba-diving and swimming". The European Respiratory Journal. 8 (5): 762–7. PMID 7656948.
- Henckes, A; Lion, F; Cochard, G; Arvieux, J; Arvieux, C (2008). "L'œdème pulmonaire en plongée sous-marine autonome : fréquence et gravité à propos d'une série de 19 cas" [Pulmonary oedema in scuba-diving: frequency and seriousness about a series of 19 cases]. Annales Françaises d'Anesthésie et de Réanimation (in French). 27 (9): 694–9. doi:10.1016/j.annfar.2008.05.011. PMID 18674877.
- Liner, M. H.; Andersson, J. P. A. (2008). "Pulmonary edema after competitive breath-hold diving". Journal of Applied Physiology. 104 (4): 986–90. CiteSeerX 10.1.1.528.4523. doi:10.1152/japplphysiol.00641.2007. PMID 18218906.
- Boussuges, A.; Pinet, C.; Thomas, P.; Bergmann, E.; Sainty, J-M.; Vervloet, D. (1999). "Haemoptysis after breath-hold diving". European Respiratory Journal. 13 (3): 697–9. doi:10.1183/09031936.99.13369799. PMID 10232449.
- Weiler-Ravell, D; Shupak, A; Goldenberg, I; Halpern, P; Shoshani, O; Hirschhorn, G; Margulis, A (1995). "Pulmonary oedema and haemoptysis induced by strenuous swimming". BMJ. 311 (7001): 361–2. doi:10.1136/bmj.311.7001.361. PMC 2550430. PMID 7640542.
- Adir, Y.; Shupak, A; Gil, A; Peled, N; Keynan, Y; Domachevsky, L; Weiler-Ravell, D (2004). "Swimming-Induced Pulmonary Edema: Clinical Presentation and Serial Lung Function". Chest. 126 (2): 394–9. doi:10.1378/chest.126.2.394. PMID 15302723.
- Koehle, Michael S; Lepawsky, Michael; McKenzie, Donald C (2005). "Pulmonary Oedema of Immersion". Sports Medicine. 35 (3): 183–90. doi:10.2165/00007256-200535030-00001. PMID 15730335.
- Yoder, JA; Viera, AJ (2004). "Management of swimming-induced pulmonary edema". American Family Physician. 69 (5): 1046, 1048–9. PMID 15023003.
- Graveline DE, Jackson MM (May 1962). "Diuresis associated with prolonged water immersion". J Appl Physiol. 17 (3): 519–24. doi:10.1152/jappl.1962.17.3.519. PMID 13901268.
- Epstein M (June 1984). "Water immersion and the kidney: implications for volume regulation". Undersea Biomed Res. 11 (2): 113–21. PMID 6567431. Retrieved 4 July 2008.
- Knight DR, Horvath SM (May 1990). "Immersion diuresis occurs independently of water temperatures in the range 25 degrees-35 degrees C". Undersea Biomed Res. 17 (3): 255–6. PMID 2356595. Retrieved 4 July 2008.
- The Review - The Bath citing Drs.J. P. O'Hare, Audrey Heywood
- Lanphier, EH (1955). "Nitrogen-Oxygen Mixture Physiology, Phases 1 and 2". US Navy Experimental Diving Unit Technical Report. AD0784151. Retrieved 10 June 2008.
- Lanphier EH, Lambertsen CJ, Funderburk LR (1956). "Nitrogen-Oxygen Mixture Physiology – Phase 3. End-Tidal Gas Sampling System. Carbon Dioxide Regulation in Divers. Carbon Dioxide Sensitivity Tests". US Navy Experimental Diving Unit Technical Report. AD0728247. Retrieved 10 June 2008.
- Lanphier EH (1958). "Nitrogen-oxygen mixture physiology. Phase 4. Carbon Dioxide sensitivity as a potential means of personnel selection. Phase 6. Carbon Dioxide regulation under diving conditions". US Navy Experimental Diving Unit Technical Report. AD0206734. Retrieved 10 June 2008.
- Lanphier EH (1956). "Nitrogen-Oxygen Mixture Physiology. Phase 5. Added Respiratory Dead Space (Value in Personnel Selection tests) (Physiological Effects Under Diving Conditions)". US Navy Experimental Diving Unit Technical Report. AD0725851. Retrieved 10 June 2008.
- Lambertsen, C. J. (1971). "Carbon Dioxide Tolerance and Toxicity". Environmental Biomedical Stress Data Center, Institute for Environmental Medicine, University of Pennsylvania Medical Center. Philadelphia, PA. IFEM Report No. 2–71. Retrieved 10 June 2008.
- Glatte Jr H. A.; Motsay G. J.; Welch B. E. (1967). "Carbon Dioxide Tolerance Studies". Brooks AFB, TX School of Aerospace Medicine Technical Report. SAM-TR-67-77. Retrieved 10 June 2008.
- Austin CC, Ecobichon DJ, Dussault G, Tirado C (December 1997). "Carbon monoxide and water vapor contamination of compressed breathing air for firefighters and divers". Journal of Toxicology and Environmental Health. 52 (5): 403–423. doi:10.1080/00984109708984073. PMID 9388533.
- Kizer, KW; Golden, JA (1987). "Lipoid pneumonitis in a commercial abalone diver". Undersea Biomedical Research. 14 (6): 545–52. PMID 3686744.
- Marx, John (2010). Rosen's emergency medicine: concepts and clinical practice (7th ed.). Philadelphia, PA: Mosby/Elsevier. p. 1870. ISBN 978-0-323-05472-0.
- Sterba, JA (1990). "Field Management of Accidental Hypothermia during Diving". US Navy Experimental Diving Unit Technical Report. NEDU-1-90. Retrieved 11 June 2008.
- Stinton, R. T. (2006). Lang, M. A.; Smith, N. E. (eds.). "Survey of Thermal Protection Strategies". Proceedings of Advanced Scientific Diving Workshop: February 23–24, 2006. Washington, DC.: Smithsonian Institution.
- Benson, AJ (2002). "35". Motion Sickness. In: Medical Aspects of Harsh Environments. 2. Washington, DC. Archived from the original (PDF) on 11 January 2009. Retrieved 9 May 2008.
- Benson, Alan J. (2002). "Motion Sickness" (PDF). In Kent B. Pandoff; Robert E. Burr (eds.). Medical Aspects of Harsh Environments. 2. Washington, D.C.: Borden Institute. pp. 1048–1083. ISBN 978-0-16-051184-4. Archived from the original (PDF) on 16 September 2012. Retrieved 4 December 2012.
- Barsky, Steven (2007). Diving in High-Risk Environments (4th ed.). Ventura, California: Hammerhead Press. ISBN 978-0-9674305-7-7.
- Robbs, Maureen (Winter 2014). "Temporomandibular Joint Dysfunction in Diving". Alert Diver. Divers Alert Network. Retrieved 28 February 2017.
- Ernest S Campbell, MD, FACS. "HBO...Indications, contraindications, links references". Scuba-doc.com. Retrieved 16 March 2013.
- "uhms.org". uhms.org. 4 January 2013. Retrieved 16 March 2013.
- Edge, C. J.; St Leger Dowse, M; Bryson, P (2005). "Scuba diving with diabetes mellitus--the UK experience 1991-2001". Undersea & Hyperbaric Medicine. 32 (1): 27–37. PMID 15796312.
- St Leger Dowse, M; Gunby, A; Moncad, R; Fife, C; Bryson, P (2006). "Scuba diving and pregnancy: Can we determine safe limits?". Journal of Obstetrics & Gynaecology. 26 (6): 509–13. doi:10.1080/01443610600797368. PMID 17000494.