Gendered impact of the COVID-19 pandemic
Coronavirus disease 2019 affects men and women differently both in terms of the outcome of infection and the effect of the disease upon society.[1] The mortality due to COVID-19 is significantly higher in men.[2] Slightly more men than women contract COVID with a ratio of 1:0.9.[2]
| Part of a series on the |
| COVID-19 pandemic |
|---|
 |
|
|
|
When looking at the socio-cultural impacts of the response to the pandemic: school closures, lockdowns and reduced access to healthcare following the COVID-19 pandemic may differentially affect the genders and possibly exaggerate existing gender disparities.[1][3][4]
Sex differences in mortality
Viral diseases affect the genders differently. Research has shown that viral illnesses like Ebola, HIV, influenza and SARS affect men and women differently. [5]
More men than women die after being affected by COVID-19.[2] The highest risk for men is in their 50s, with the gap between men and women closing only at 90.[6] In China, the death rate was 2.8 percent for men and 1.7 percent for women.[6]
The reasons for this difference are not known, but genetic, social, and behavioral factors may play a part.[1][7] Sex-based immunological differences, lesser prevalence of smoking in women and men developing co-morbid conditions such as hypertension at a younger age than women could have contributed to the higher mortality in men.[6] In Europe, 57% of the infected individuals were men and 72% of those died with COVID-19 were men.[8] As of April 2020, the US government is not tracking sex-related data of COVID-19 infections.[5]
Impact on health
Women as caregivers
Globally, women do three times as much unpaid care work as men.[9][10][11] Evidence from past disease outbreaks show that a greater burden is placed on care in the home and that women are more likely to be caregivers for the sick individuals in the family, making them more vulnerable to infection.[1][12][13]
Women in medical roles
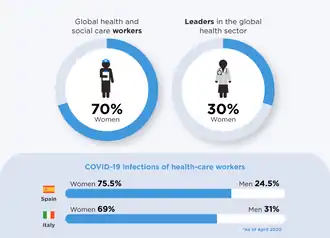
Globally, women make up 70 percent of workers in the health and social sector. 90% of the healthcare workers in China's Hubei province (where the disease originated) were women and 78% of the healthcare workers in the USA are women.[13] Women are playing a disproportionate role in responding to the disease, including as front line healthcare workers (as well as caregivers at home and community leaders and mobilisers). In some countries, COVID-19 infections among female health workers are twice that of their male counterparts.[9][10][11] Women are still paid much less than their male counterparts in almost all countries and hold fewer leadership positions in the health sector. Masks and other protective equipment designed and sized for men leave women at greater risk of exposure.[9][10][11]
Access to healthcare
Women and girls, who already faced health and safety implications in managing their sexual and reproductive health and menstrual hygiene without access to clean water and private toilets before the crisis, are particularly in danger. When healthcare systems are overburdened and resources are reallocated to respond to the pandemic, this can further disrupt health services unique to the well-being of women and girls. This includes pre- and post-natal healthcare, access to quality sexual and reproductive health services, and life-saving care and support for survivors of gender-based violence.[9][14][15][16] Women are also refraining from visiting health facilities due to fears about COVID-19 exposure or due to movement restrictions.[17] The health impacts can be catastrophic, especially in rural, marginalized and low-literacy communities, where women are less likely to have access to quality, culturally-accessible health services, essential medicines or insurance coverage. Before the pandemic, around 810 women died every day from preventable causes related to pregnancy and childbirth—94 per cent of these deaths occurred in low and lower middle-income countries. Past pandemics have shown increased rates of maternal mortality and morbidity, adolescent pregnancies, and HIV and other sexually transmitted diseases. Multiple and intersecting inequalities, such as ethnicity, socioeconomic status, disability, age, race, geographic location and sexual orientation, among others, can further compound these impacts.[9][14][15][16]
Reproductive health
During an outbreak, healthcare resources are diverted to combat the disease, which results in down-prioritizing reproductive health of women.[18][19] The physiological changes in pregnancy puts women at an increased risk for some infections, although evidence is lacking particularly about COVID-19. Women had a higher risk of developing severe illness when affected with influenza virus (which belongs to the same family as COVID-19), so it is important to protect pregnant women from being infected with COVID-19.[20] Women nurses were reported to have decreased access to tampons and sanitary pads while also working overtime without adequate personal protective equipment during the COVID-19 pandemic in mainland China.[21] Various researchers have speculated that coronavirus may harm male fertility, either from direct viral effects or from the immune response inflammation.[22]
Contraceptives
Supply chain disruptions are limiting availability of contraceptives in many places, and stock-outs of many contraceptive methods are anticipated within the next 6 months in more than a dozen lowest- income countries by UNFPA.[17] Product shortages and lack of access to trained providers or clinics mean that women may be unable to use their preferred method of contraception, may instead use a less effective short-term method, or may discontinue contraceptive use entirely. 47 million women in 114 low and middle-income countries are projected by UNFPA to be unable to use modern contraceptives if the average lockdown, or COVID-19-related disruption, continues for 6 months with major disruptions to services: For every 3 months the lockdown continues, assuming high levels of disruption, up to 2 million additional women may be unable to use modern contraceptives. If the lockdown continues for 6 months and there are major service disruptions due to COVID-19, an additional 7 million unintended pregnancies are expected to occur by UNFPA. The number of unintended pregnancies will increase as the lockdown continues and services disruptions are extended.[23] Reduced access is likely to more adversely affect younger, poorer and more vulnerable and marginalized populations.[17]
Abortion policies
The government of Argentina was planning to submit a bill to the Congress to grant abortion rights to women in March, after the official announcement of president Alberto Fernández in his speech opening the Congress sessions on March, 1.[24] However, the submission of the bill was postponed due to the coronavirus crisis and the lock down of the country.[25] Provision of abortion services under the current law is still being granted in the country,[26] albeit with challenges due to some provinces that have historically opposed abortion. The Ministry of Women of Argentina is working to facilitate abortion through the establishment of a helpline that women can call to obtain information.[27] In December 2020, Argentina passed legislation to legally allow abortion.[28]
Clinical trials
Women are underrepresented in clinical trials for vaccines and drugs, as a result of which sex-differences in disease response could be ignored in scientific studies.[5]
Nutrition
During public health emergencies, women are at an increased risk of malnutrition.[29]
Socio-economic impact

Women constitute a larger part of informal and part-time workers around the world. During periods of uncertainty, such as during a pandemic, women are at a greater risk of being unemployed and being unable to return to work after the pandemic is over.[13] Quarantine experience can be different for men and women, considering the difference in physical, cultural, security and sanitary needs for both genders.[30]
Domestic workers
Domestic work is largely dominated by women and has important levels of informality.[31] In particular, migrant domestic workers are in a more vulnerable situation, with unclear immigration status and lack of legal protection. In situations where those migrant domestic workers come from less-developed countries, their families back home are dependent of their remittance to survive in the country of origin of the worker. In Philippines, those remittances account for 9% of their GDP, therefore impacting their country of origin's economy.[32] In Argentina, they have established a unique-payment for all domestic workers, and childcare and elderly care is deemed an essential activity so they are allowed to circulate even with the lock down.[33]
The U.S. Congress included $3.5 billion in grants for childcare providers in the CARES Act in March 2020. However, this is insufficient to sustain most childcare providers who have lost work. The Center for Law And Policy estimated that childcare providers in the United States will need $9.6 billion per month to economically survive the effects of a hypothetical six-month period of reduced activity.[34]
Increase in unpaid care work
Before the crisis started, women did nearly three times as much unpaid care and domestic work as men. Social distancing measures, school closures and overburdened health systems have put an increased demand on women and girls to cater to the basic survival needs of the family and care for the sick and the elderly. With more than 1.5 billion students at home as of March 2020 due to the pandemic, existing gender norms have put the increased demand for unpaid childcare and domestic work on women.[9][10][35][36][37][38][39][40][41] This constrains their ability to carry out paid work, particularly when jobs cannot be carried out remotely. The lack of childcare support is particularly problematic for essential workers and lone mothers who have care responsibilities. Discriminatory social norms are likely to increase the unpaid work load of COVID-19 on girls and adolescent girls, especially those living in poverty or in rural, isolated locations. Evidence from past epidemics shows that adolescent girls are at particular risk of dropping out and not returning to school even after the crisis is over. Women's unpaid care work has long been recognized as a driver of inequality with direct links to wage inequality, lower income, and physical and mental health stressors. As countries rebuild economies, the crisis might offer an opportunity to recognize, reduce and redistribute unpaid care work once and for all.[9][10][35][36][37][38][39][40][41]
Gender based violence

Due to increased tension in the household during a pandemic, women and girls are likely to experience higher risk of intimate partner violence and other forms of domestic violence.[30][42][43] In Kosovo, there has been a 17% increase in gender based violence during the pandemic.[44] During periods of lockdown, women experiencing domestic violence have limited access to protective services.[29][45] In Sint Maarten, the sale of alcohol was temporarily halted to prevent more domestic violence from occurring.[46]
References
- Wenham, Clare; Smith, Julia; Morgan, Rosemary (14 March 2020). "COVID-19: the gendered impacts of the outbreak". The Lancet. 395 (10227): 846–848. doi:10.1016/S0140-6736(20)30526-2. ISSN 0140-6736. PMC 7124625. PMID 32151325. Archived from the original on 10 April 2020. Retrieved 7 April 2020.
- Ortolan, Augusta; Lorenzin, Mariagrazia; Felicetti, Mara; Doria, Andrea; Ramonda, Roberta (2020-10-01). "Does gender influence clinical expression and disease outcomes in COVID-19? A systematic review and meta-analysis". International Journal of Infectious Diseases. 99: 496–504. doi:10.1016/j.ijid.2020.07.076. ISSN 1201-9712. PMC 7422797. PMID 32800858.
- "Gender and the Coronavirus Outbreak: Think Global Health". Council on Foreign Relations. Archived from the original on 10 April 2020. Retrieved 7 April 2020.
- Aristovnik A, Keržič D, Ravšelj D, Tomaževič N, Umek L (October 2020). "Impacts of the COVID-19 Pandemic on Life of Higher Education Students: A Global Perspective". Sustainability. 12 (20): 8438. doi:10.3390/su12208438.
- Gupta, Alisha Haridasani (3 April 2020). "Does Covid-19 Hit Women and Men Differently? U.S. Isn't Keeping Track". The New York Times. Archived from the original on 10 April 2020. Retrieved 7 April 2020.
- Rabin, Roni Caryn (20 March 2020). "In Italy, Coronavirus Takes a Higher Toll on Men". The New York Times. Archived from the original on 10 April 2020. Retrieved 7 April 2020.
- Sharma Garima; Volgman Annabelle Santos; Michos Erin D. (2020-07-15). "Sex Differences in Mortality From COVID-19 Pandemic". JACC: Case Reports. 2 (9): 1407–1410. doi:10.1016/j.jaccas.2020.04.027. PMC 7198137. PMID 32373791.
- "COVID-19 weekly surveillance report". www.euro.who.int. Archived from the original on 10 April 2020. Retrieved 7 April 2020.
- "UN Secretary-General's policy brief: The impact of COVID-19 on women | Digital library: Publications". UN Women. Archived from the original on 2020-06-10. Retrieved 2020-06-12.
- "Gender equality matters in COVID-19 response". UN Women. Archived from the original on 2020-06-13. Retrieved 2020-06-12.
- "COVID-19: Emerging gender data and why it matters | UN Women Data Hub". data.unwomen.org. Archived from the original on 2020-06-12. Retrieved 2020-06-12.
- Davies, Sara E.; Bennett, Belinda (2016). A gendered human rights analysis of Ebola and Zika: locating gender in global health emergencies. pp. 1041–1060. Archived from the original on 7 April 2020. Retrieved 7 April 2020.
- Gupta, Alisha Haridasani (12 March 2020). "Why Women May Face a Greater Risk of Catching Coronavirus". The New York Times. Archived from the original on 10 April 2020. Retrieved 7 April 2020.
- "WHO | Progress on drinking water, sanitation and hygiene". WHO. Archived from the original on 2020-07-07. Retrieved 2020-07-01.
- "Home | JMP". washdata.org. Archived from the original on 2020-07-05. Retrieved 2020-07-01.
- "Menstrual Hygiene Management Enables Women and Girls to Reach Their Full Potential". World Bank. Archived from the original on 2019-10-14. Retrieved 2020-07-01.
- "Impact of the COVID-19 Pandemic on Family Planning and Ending Gender-based Violence, Female Genital Mutilation and Child Marriage". www.unfpa.org. Archived from the original on 2020-06-23. Retrieved 2020-06-24.
- Rimmer, MP; Al Wattar, BH; UKARCOG Members (2020-05-27). "Provision of obstetrics and gynaecology services during the COVID‐19 pandemic: a survey of junior doctors in the UK National Health Service". BJOG: An International Journal of Obstetrics & Gynaecology. 127 (9): 1471–0528.16313. doi:10.1111/1471-0528.16313. ISSN 1470-0328. PMC 7283977. PMID 32460422.
- Sochas, Laura; Channon, Andrew Amos; Nam, Sara (2017). Counting indirect crisis-related deaths in the context of a low-resilience health system: the case of maternal and neonatal health during the Ebola epidemic in Sierra Leone. pp. iii32–iii39. Archived from the original on 7 April 2020. Retrieved 7 April 2020.
- "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 7 April 2020. Retrieved 7 April 2020.
- Stevenson, Alexandra (26 February 2020). "Shaved Heads, Adult Diapers: Life as a Nurse in the Coronavirus Outbreak". The New York Times. Archived from the original on 10 April 2020. Retrieved 7 April 2020.
- Huang, Chuan; Ji, Xiren; Zhou, Wenjun; Huang, Zhenghui; Peng, Xiangjie; Fan, Liqing; Lin, Ge; Zhu, Wenbing (2020). "Coronavirus: A possible cause of reduced male fertility". Andrology. American Society of Andrology and European Academy of Andrology. doi:10.1111/andr.12907. PMC 7537192. PMID 32960504. Retrieved 23 October 2020.
- Impact of the COVID-19 Pandemic on Family Planning and Ending Gender-based Violence, Female Genital Mutilation and Child Marriage (PDF). UNFPA. 2020. Archived (PDF) from the original on 2020-08-17. Retrieved 2020-09-25.
- Página12. "Aborto y otras definiciones centrales de Alberto Fernández en la apertura de sesiones ordinarias 2020 | Lo principal del discurso del Presidente en el Congreso". PAGINA12. Archived from the original on 2020-03-14. Retrieved 2020-04-14.
- Clarín.com. "Por el coronavirus, el Gobierno analiza dilatar el envío al Congreso de dos proyectos clave: aborto legal y reforma judicial". www.clarin.com (in Spanish). Archived from the original on 2020-04-22. Retrieved 2020-04-14.
- Página12. "¿Cómo abortar en época de cuarentena por coronavirus? | Otras urgencias de la salud pública". PAGINA12. Archived from the original on 2020-04-01. Retrieved 2020-04-14.
- Beck, Ingrid. "Abortar en tiempos de coronavirus". Letra P (in Spanish). Archived from the original on 2020-06-06. Retrieved 2020-04-14.
- "Cross-post: An Intersectional Approach to a Pandemic? Gender Data, Disaggregation, and COVID-19". Digital Impact Alliance. Archived from the original on 10 April 2020. Retrieved 7 April 2020.
- "COVID-19: A Gender Lens". www.unfpa.org. Archived from the original on 10 April 2020. Retrieved 7 April 2020.
- "New strategies to reduce informality in domestic work". www.ilo.org. 2016-12-05. Archived from the original on 2020-05-20. Retrieved 2020-04-14.
- Owen, Lara (2020-03-08). "Five ways the coronavirus is hitting women in Asia". BBC News. Archived from the original on 2020-04-14. Retrieved 2020-04-14.
- "Coronavirus: qué pasa con las niñeras y trabajadoras domésticas en la cuarentena total". El Cronista (in Spanish). Archived from the original on 2020-06-06. Retrieved 2020-04-14.
- Peck, Emily (2020-05-15). "The Child Care Industry Is About To Collapse. There's No Bailout Coming". HuffPost. Archived from the original on 2020-05-15. Retrieved 2020-05-15.
- "Coronavirus puts women in the frontline". European Institute for Gender Equality. Archived from the original on 2020-04-11. Retrieved 2020-04-14.
- "Unpaid care work: Your load and why it matters". interactive.unwomen.org. Retrieved 2020-07-01.
- "Spotlight on SDG 8: The impact of marriage and children on labour market participation | Digital library: Publications". UN Women. Archived from the original on 2020-06-29. Retrieved 2020-07-01.
- https://plus.google.com/+UNESCO (2020-03-31). "Covid-19 school closures around the world will hit girls hardest". UNESCO. Archived from the original on 2020-06-27. Retrieved 2020-07-01.
- https://plus.google.com/+UNESCO (2020-03-04). "Education: From disruption to recovery". UNESCO. Archived from the original on 2020-03-31. Retrieved 2020-07-01.
- UN Women. (19 September 2019). Families in a changing world / UN Women. New York. ISBN 978-1-63214-156-9. OCLC 1120137550.
- Women, U. N. "How COVID-19 impacts women and girls". interactive.unwomen.org. Archived from the original on 2020-06-28. Retrieved 2020-07-01.
- "Gender Equality and Addressing Gender-based Violence (GBV) and Coronavirus Disease (COVID-19) Prevention, Protection and Response". www.unfpa.org. Archived from the original on 10 April 2020. Retrieved 7 April 2020.
- "UN chief calls for domestic violence 'ceasefire' amid 'horrifying global surge'". UN News. 2020-04-05. Archived from the original on 2020-04-10. Retrieved 2020-04-07.
- "Gender-based violence spikes amid pandemic, shelters need support". www.unfpa.org. Archived from the original on 10 April 2020. Retrieved 7 April 2020.
- "How Coronavirus Is Affecting Victims of Domestic Violence". Time. Archived from the original on 10 April 2020. Retrieved 7 April 2020.
- "Alcoholverbod Sint Maarten door stijging huiselijk geweld tijdens lockdown". Telegraaf (in Dutch). 13 April 2020. Archived from the original on 6 June 2020. Retrieved 20 April 2020.
![]() This article incorporates text from a free content work. Licensed under CC BY-SA 3.0 IGO License statement/permission on Wikimedia Commons. Text taken from Explainer: How COVID-19 impacts women and girls, UN Women.
This article incorporates text from a free content work. Licensed under CC BY-SA 3.0 IGO License statement/permission on Wikimedia Commons. Text taken from Explainer: How COVID-19 impacts women and girls, UN Women.
Further reading
- Griffith DM, Sharma G, Holliday CS, Enyia OK, Valliere M, Semlow AR, et al. (July 2020). "Men and COVID-19: A Biopsychosocial Approach to Understanding Sex Differences in Mortality and Recommendations for Practice and Policy Interventions" (PDF). Prev Chronic Dis. 17: E63. doi:10.5888/pcd17.200247. PMC 7380297. PMID 32678061.
- Peckham H, de Gruijter NM, Raine C, Radziszewska A, Ciurtin C, Wedderburn LR, et al. (December 2020). "Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission". Nature Communications volume. 11 (6317). doi:10.1038/s41467-020-19741-6.
External links
- Rajewski, Genevieve (15 June 2020). "Why Is There a COVID-19 Gender Gap?". Tufts Now.
- Reeves RV, Ford TN (15 May 2020). "COVID-19 much more fatal for men, especially taking age into account". The Brookings Institution.