Symptoms of COVID-19
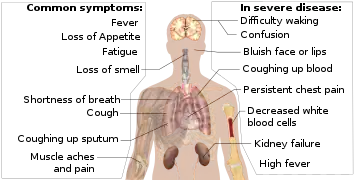
Symptoms of COVID-19 are variable, ranging from mild symptoms to severe illness.[1][2] Common symptoms include headache, loss of smell and taste, nasal congestion and rhinorrhea, cough, muscle pain, sore throat, fever, and breathing difficulties.[3] People with the same infection may have different symptoms, and their symptoms may change over time. In people without prior ears, nose, and throat disorders, loss of taste combined with loss of smell is associated with COVID-19 with a specificity of 95%.[4]
| Part of a series on the |
| COVID-19 pandemic |
|---|
 |
|
|
|
Most people (81%) develop mild to moderate symptoms (up to mild pneumonia), while 14% develop severe symptoms (dyspnea, hypoxia, or more than 50% lung involvement on imaging) and 5% of patients suffer critical symptoms (respiratory failure, shock, or multiorgan dysfunction).[5] At least a third of the people who are infected with the virus do not develop noticeable symptoms at any point in time.[6][7][8][9] These asymptomatic carriers tend not to get tested and can spread the disease.[9][10][11][12] Other infected people will develop symptoms later, called "pre-symptomatic", or have very mild symptoms and can also spread the virus.[13]
As is common with infections, there is a delay between the moment a person first becomes infected and the appearance of the first symptoms. The median delay for COVID-19 is four to five days.[14] Most symptomatic people experience symptoms within two to seven days after exposure, and almost all will experience at least one symptom within 12 days.[14][15]
Most people recover from the acute phase of the disease. However, some patients continue to experience a range of effects for months after recovery—named long COVID—and damage to organs has been observed. Multi-year studies are underway to further investigate the long-term effects of the disease.[16]
Initial symptoms
Some symptoms of COVID-19 can be relatively non-specific; the two most common symptoms are fever (88 percent) and dry cough (68 percent).[17][18] Among those who develop symptoms, approximately one in five may become more seriously ill and have difficulty in breathing. Emergency symptoms include difficulty breathing, persistent chest pain or pressure, sudden confusion, difficulty waking, and bluish face or lips; immediate medical attention is advised if these symptoms are present.[18] Further development of the disease can lead to complications including pneumonia, acute respiratory distress syndrome, sepsis, septic shock, and kidney failure.
Some symptoms usually appear sooner than others. In August 2020, scientists at the University of Southern California reported the "likely" order of initial symptoms of the COVID-19 disease as a fever followed by a cough and muscle pain, and that nausea and vomiting usually appear before diarrhea.[19] This contrasts with the most common path for influenza where it is common to develop a cough first and fever later.[19]
Fever
Fever is the most common symptom of COVID-19.[2] The fever may be high or low. Most people with COVID-19 develop a fever at some point.[2]
Respiratory
Most people with COVID-19 also have a cough, which could be either dry or a productive cough.[2]
Some symptoms, such as difficulty breathing, are more common in patients who need hospital care.[1] Shortness of breath tends to develop later in the illness.
Loss of smell or taste
About 40% of people temporarily lose their sense of smell (called anosmia), experience changes in how food tastes (dysgeusia), or have other disturbances to their normal abilities to smell or taste.[1][20] This symptom, if it is present at all, often appears early in the illness. A disturbance in smell or taste is more commonly found in younger people, and perhaps because of this, it is associated with a lower risk of medical complications. Although the majority of people with COVID-19 do not experience these symptoms, it is an unusual symptom for other respiratory diseases, so it is used for symptom-based screening.[20]
Neurological symptoms
Patients with COVID-19 can present with neurological symptoms that can be broadly divided into central nervous system involvement, such as headache, dizziness, altered mental state, and disorientation, and peripheral nervous system involvement, such as anosmia and dysgeusia.[21] Some patients experience cognitive dysfunction called "COVID fog", or "COVID brain fog", involving memory loss, inattention, poor concentration or disorientation.[22][23]
Skin rashes

Various skin rashes have been observed in COVID-19 patients, including morbilliform rash, livedo reticularis, and vesicular blisters.[24] The so-called "COVID toes" are pink to violaceous papules arising on the hands and feet. These chilblain-like lesions often occur only in younger patients and do not appear until late in the disease or during convalescence.[25]
Other
Other typical symptoms include fatigue, and muscle and joint pains.[1][2][17][18]
Other symptoms are less common among people with COVID-19. Some people experience gastrointestinal symptoms such as loss of appetite, diarrhea, nausea or vomiting.[1][26] Some people have a sore throat, headache, or vertigo.[1][2][17][18] Less common symptoms include chills, coughing out blood, diarrhea, and rash.[17][18]
Complications
Complications may include pneumonia, acute respiratory distress syndrome (ARDS), multi-organ failure, septic shock, and death.[27][28][29][30] Cardiovascular complications may include heart failure, arrhythmias, heart inflammation, and blood clots.[31][32][33][34] Approximately 20–30% of people who present with COVID-19 have elevated liver enzymes, reflecting liver injury.[35][36]
Neurologic manifestations include seizures, strokes, encephalitis, and Guillain–Barré syndrome (which includes loss of motor functions).[37][38] Following the infection, children may develop paediatric multisystem inflammatory syndrome, which has symptoms similar to Kawasaki disease, which can be fatal.[39][40][41]
Longer-term effects
Some early studies suggest that between one in five and one in 10 people with COVID-19 will experience symptoms lasting longer than a month.[42][43] A majority of those who were admitted to hospital with severe disease report long-term problems, including fatigue and shortness of breath.[44] About 5-10% of patients admitted to hospital progress to severe or critical disease, including pneumonia and acute respiratory failure.[45]
References
- "Symptoms of Coronavirus". U.S. Centers for Disease Control and Prevention (CDC). 13 May 2020. Archived from the original on 17 June 2020. Retrieved 18 June 2020.
- Grant MC, Geoghegan L, Arbyn M, Mohammed Z, McGuinness L, Clarke EL, Wade RG (23 June 2020). "The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS-CoV-2; COVID-19): A systematic review and meta-analysis of 148 studies from 9 countries". PLOS ONE. 15 (6): e0234765. Bibcode:2020PLoSO..1534765G. doi:10.1371/journal.pone.0234765. PMC 7310678. PMID 32574165. S2CID 220046286.
- "Clinical characteristics of COVID-19". European Centre for Disease Prevention and Control. Retrieved 2020-12-29.
- Bénézit, François; Le Turnier, Paul; Declerck, Charles; Paillé, Cécile; Revest, Matthieu; Dubée, Vincent; Tattevin, Pierre (2020). "Utility of hyposmia and hypogeusia for the diagnosis of COVID-19". The Lancet Infectious Diseases. 20 (9): 1014–1015. doi:10.1016/S1473-3099(20)30297-8. PMC 7159866. PMID 32304632. S2CID 215769604.
- "Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 6 April 2020. Archived from the original on 2 March 2020. Retrieved 19 April 2020.
- Oran, Daniel P.; Topol, Eric J. (2021-01-22). "The Proportion of SARS-CoV-2 Infections That Are Asymptomatic". Annals of Internal Medicine. doi:10.7326/M20-6976. ISSN 0003-4819. PMC 7839426.
- "Transmission of COVID-19". European Centre for Disease Prevention and Control. Retrieved 2020-12-06.
- Nogrady, Bianca (2020-11-18). "What the data say about asymptomatic COVID infections". Nature. 587 (7835): 534–535. doi:10.1038/d41586-020-03141-3. PMID 33214725.
- Gao Z, Xu Y, Sun C, Wang X, Guo Y, Qiu S, Ma K (May 2020). "A Systematic Review of Asymptomatic Infections with COVID-19". Journal of Microbiology, Immunology, and Infection = Wei Mian Yu Gan Ran Za Zhi. doi:10.1016/j.jmii.2020.05.001. PMC 7227597. PMID 32425996.
- Oran, Daniel P., and Eric J. Topol. “Prevalence of Asymptomatic SARS-CoV-2 Infection : A Narrative Review.” Annals of Internal Medicine. vol. 173,5 (2020): 362-367. doi:10.7326/M20-3012 PMID: 32491919 Retrieved 14 January 2021.
- Lai CC, Liu YH, Wang CY, Wang YH, Hsueh SC, Yen MY, et al. (June 2020). "Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): Facts and myths". Journal of Microbiology, Immunology, and Infection = Wei Mian Yu Gan Ran Za Zhi. 53 (3): 404–412. doi:10.1016/j.jmii.2020.02.012. PMC 7128959. PMID 32173241.
- Furukawa NW, Brooks JT, Sobel J (July 2020). "Evidence Supporting Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 While Presymptomatic or Asymptomatic". Emerging Infectious Diseases. 26 (7). doi:10.3201/eid2607.201595. PMC 7323549. PMID 32364890.
- Furukawa, Nathan W.; Brooks, John T.; Sobel, Jeremy (4 May 2020). "Evidence Supporting Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 While Presymptomatic or Asymptomatic". Emerging Infectious Diseases. 26 (7). doi:10.3201/eid2607.201595. PMC 7323549. PMID 32364890. Retrieved 29 September 2020.
- Gandhi RT, Lynch JB, Del Rio C (April 2020). "Mild or Moderate Covid-19". The New England Journal of Medicine. 383 (18): 1757–1766. doi:10.1056/NEJMcp2009249. PMID 32329974.
- Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC (August 2020). "Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review". JAMA. 324 (8): 782–793. doi:10.1001/jama.2020.12839. PMID 32648899. S2CID 220465311.
- CDC (2020-02-11). "COVID-19 and Your Health". Centers for Disease Control and Prevention. Retrieved 2021-01-23.
- "Coronavirus". World Health Organization (WHO). Retrieved 4 May 2020.
- "Symptoms of Coronavirus". U.S. Centers for Disease Control and Prevention (CDC). 20 March 2020. Archived from the original on 30 January 2020.
- Larsen JR, Martin MR, Martin JD, Kuhn P, Hicks JB (13 August 2020). "Modeling the Onset of Symptoms of COVID-19". Frontiers in Public Health. 8: 473. doi:10.3389/fpubh.2020.00473. PMC 7438535. PMID 32903584. S2CID 221105179.
- Agyeman AA, Chin KL, Landersdorfer CB, Liew D, Ofori-Asenso R (August 2020). "Smell and Taste Dysfunction in Patients With COVID-19: A Systematic Review and Meta-analysis". Mayo Clinic Proceedings. 95 (8): 1621–1631. doi:10.1016/j.mayocp.2020.05.030. PMC 7275152. PMID 32753137.
- Payus, Alvin Oliver; Lin, Constance Liew Sat; Noh, Malehah Mohd; Jeffree, Mohammad Saffree; Ali, Raymond Azman (2020-08-03). "SARS-CoV-2 infection of the nervous system: A review of the literature on neurological involvement in novel coronavirus disease-(COVID-19)". Bosnian Journal of Basic Medical Sciences. 20 (3): 283–292. doi:10.17305/bjbms.2020.4860. ISSN 1840-4812. PMC 7416180. PMID 32530389.
- Even Mild Cases Can Cause "COVID-19 Fog", Columbia University Irving Medical Center, September 21, 2020
- Pam Belluck (October 11, 2020), "How Brain Fog Plagues Covid-19 Survivors", The New York Times
- https://dermnetnz.org/topics/covid-19/
- Massey, Paul (23 May 2020). "Going viral: A brief history of Chilblain-like skin lesions ("COVID toes") amidst the COVID-19 pandemic". Semin Oncol. 47 (5): 330–334. doi:10.1053/j.seminoncol.2020.05.012. PMC 7245293. PMID 32736881.
- Berlin DA, Gulick RM, Martinez FJ (May 2020). Solomon CG (ed.). "Severe Covid-19". The New England Journal of Medicine. 383 (25): 2451–2460. doi:10.1056/NEJMcp2009575. PMID 32412710. S2CID 218649520.
- Hui DS, I Azhar E, Madani TA, Ntoumi F, Kock R, Dar O, et al. (February 2020). "The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health – The latest 2019 novel coronavirus outbreak in Wuhan, China". International Journal of Infectious Diseases. 91: 264–266. doi:10.1016/j.ijid.2020.01.009. PMC 7128332. PMID 31953166.
- Murthy S, Gomersall CD, Fowler RA (March 2020). "Care for Critically Ill Patients With COVID-19". JAMA. 323 (15): 1499–1500. doi:10.1001/jama.2020.3633. PMID 32159735.
- Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R (2020). "Features, Evaluation and Treatment Coronavirus (COVID-19)". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 32150360. Retrieved 18 March 2020.
- Heymann DL, Shindo N, et al. (WHO Scientific and Technical Advisory Group for Infectious Hazards) (February 2020). "COVID-19: what is next for public health?". Lancet. 395 (10224): 542–545. doi:10.1016/s0140-6736(20)30374-3. PMC 7138015. PMID 32061313.
- Long B, Brady WJ, Koyfman A, Gottlieb M (July 2020). "Cardiovascular complications in COVID-19". The American Journal of Emergency Medicine. 38 (7): 1504–1507. doi:10.1016/j.ajem.2020.04.048. PMC 7165109. PMID 32317203.
- Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, et al. (July 2020). "Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19)". JAMA Cardiology. 5 (11): 1265–1273. doi:10.1001/jamacardio.2020.3557. PMC 7385689. PMID 32730619. Lay summary.
- Lindner D, Fitzek A, Bräuninger H, Aleshcheva G, Edler C, Meissner K, et al. (July 2020). "Association of Cardiac Infection With SARS-CoV-2 in Confirmed COVID-19 Autopsy Cases". JAMA Cardiology. 5 (11): 1281–1285. doi:10.1001/jamacardio.2020.3551. PMC 7385672. PMID 32730555. Lay summary.
- Siripanthong, Bhurint (2020). "Recognizing COVID-19–related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management". Heart Rhythm. 17 (9): 1463–1471. doi:10.1016/j.hrthm.2020.05.001. PMC 7199677. PMID 32387246.
- Xu L, Liu J, Lu M, Yang D, Zheng X (May 2020). "Liver injury during highly pathogenic human coronavirus infections". Liver International. 40 (5): 998–1004. doi:10.1111/liv.14435. PMC 7228361. PMID 32170806.
- Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB (April 2020). "Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review". JAMA. 323 (18): 1824–1836. doi:10.1001/jama.2020.6019. PMID 32282022.
- Carod-Artal FJ (May 2020). "Neurological complications of coronavirus and COVID-19". Revista de Neurología. 70 (9): 311–322. doi:10.33588/rn.7009.2020179. PMID 32329044.
- Toscano, Gianpaolo (2020). "Guillain–Barré Syndrome Associated with SARS-CoV-2". New England Journal of Medicine. 382 (26): 2574–2576. doi:10.1056/NEJMc2009191. PMC 7182017. PMID 32302082.
- "Multisystem inflammatory syndrome in children and adolescents temporally related to COVID-19". World Health Organization (WHO). 15 May 2020. Retrieved 20 May 2020.
- HAN Archive – 00432 (Report). U.S. Centers for Disease Control and Prevention (CDC). 15 May 2020. Retrieved 20 May 2020.
- Huang, C; Wang, Y; Li, X; Ren, L; Zhao, J; Hu, Y; Zhang, L; Fan, G; Xu, J; Gu, X; Cheng, Z; Yu, T; Xia, J; Wei, Y; Wu, W; Xie, X; Yin, W; Li, H; Liu, M; Xiao, Y; Gao, H; Guo, L; Xie, J; Wang, G; Jiang, R; Gao, Z; Jin, Q; Wang, J; Cao, B (15 February 2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". Lancet. London, England: Elsevier. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. PMC 7159299. PMID 31986264.
- "Living with Covid19". NIH Themed Review. National Institute for Health Research. 15 October 2020. doi:10.3310/themedreview_41169.
- "How long does COVID-19 last?". UK COVID Symptom Study. 6 Jun 2020. Retrieved 15 Oct 2020.
- "Summary of COVID-19 Long Term Health Effects: Emerging evidence and Ongoing Investigation" (PDF). University of Washington. 1 September 2020. Retrieved 15 October 2020.
- Huang, C; Wang, Y; Li, X; Ren, L; Zhao, J; Hu, Y; Zhang, L; Fan, G; Xu, J; Gu, X; Cheng, Z; Yu, T; Xia, J; Wei, Y; Wu, W; Xie, X; Yin, W; Li, H; Liu, M; Xiao, Y; Gao, H; Guo, L; Xie, J; Wang, G; Jiang, R; Gao, Z; Jin, Q; Wang, J; Cao, B (15 February 2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". Lancet. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. PMC 7159299. PMID 31986264.