Dopamine receptor
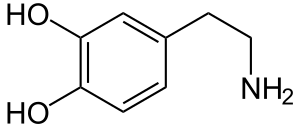
Dopamine receptors are a class of G protein-coupled receptors that are prominent in the vertebrate central nervous system (CNS). Dopamine receptors activate different effectors through not only G-protein coupling, but also signaling through different protein (dopamine receptor-interacting proteins) interactions.[1] The neurotransmitter dopamine is the primary endogenous ligand for dopamine receptors.
Dopamine receptors are implicated in many neurological processes, including motivation, pleasure, cognition, memory, learning, and fine motor control, as well as modulation of neuroendocrine signaling. Abnormal dopamine receptor signaling and dopaminergic nerve function is implicated in several neuropsychiatric disorders.[2] Thus, dopamine receptors are common neurologic drug targets; antipsychotics are often dopamine receptor antagonists while psychostimulants are typically indirect agonists of dopamine receptors.
Subtypes
The existence of multiple types of receptors for dopamine was first proposed in 1976.[3][4] There are at least five subtypes of dopamine receptors, D1, D2, D3, D4, and D5. The D1 and D5 receptors are members of the D1-like family of dopamine receptors, whereas the D2, D3 and D4 receptors are members of the D2-like family. There is also some evidence that suggests the existence of possible D6 and D7 dopamine receptors, but such receptors have not been conclusively identified.[5]
At a global level, D1 receptors have widespread expression throughout the brain. Furthermore, D1-2 receptor subtypes are found at 10-100 times the levels of the D3-5 subtypes.[6]
D1-like family
The D1-like family receptors are coupled to the G protein Gsα. D1 is also coupled to Golf.
Gsα subsequently activates adenylyl cyclase, increasing the intracellular concentration of the second messenger cyclic adenosine monophosphate (cAMP).[7]
- D1 is encoded by the Dopamine receptor D1 gene (DRD1).
- D5 is encoded by the Dopamine receptor D5 gene (DRD5).
D2-like family
The D2-like family receptors are coupled to the G protein Giα, which directly inhibits the formation of cAMP by inhibiting the enzyme adenylyl cyclase.[8]
- D2 is encoded by the Dopamine receptor D2 gene (DRD2), of which there are two forms: D2Sh (short) and D2Lh (long):
- The D2Sh form is pre-synaptically situated, having modulatory functions (viz., autoreceptors, which regulate neurotransmission via feedback mechanisms. It affects synthesis, storage, and release of dopamine into the synaptic cleft).[9]
- The D2Lh form may function as a classical post-synaptic receptor, i.e., transmit information (in either an excitatory or an inhibitory fashion) unless blocked by a receptor antagonist or a synthetic partial agonist.[9]
- D3 is encoded by the Dopamine receptor D3 gene (DRD3). Maximum expression of dopamine D3 receptors is noted in the islands of Calleja and nucleus accumbens.[10]
- D4 is encoded by the Dopamine receptor D4 gene (DRD4). The D4 receptor gene displays polymorphisms that differ in a variable number tandem repeat present within the coding sequence of exon 3.[11] Some of these alleles are associated with greater incidence of certain disorders. For example, the D4.7 alleles have an established association with attention-deficit hyperactivity disorder.[12][13][14]
Receptor heteromers
Dopamine receptors have been shown to heteromerize with a number of other G protein-coupled receptors.[15] Especially the D2 receptor is considered a major hub within the GPCR heteromer network.[16] Protomers consist of
Isoreceptors[17]
- D1–D2
- D1–D3
- D2–D3
- D2–D4
- D2–D5
Non-isoreceptors
- D1–adenosine A1
- D2–adenosine A2A
- D2–ghrelin receptor
- D2sh–TAAR1 (an autoreceptor heteromer)
- D4–adrenoceptor α1B
- D4–adrenoceptor β1
Signaling mechanism
Dopamine receptor D1 and Dopamine receptor D5 are Gs coupled receptors that stimulate adenylyl cyclase to produce cAMP, increasing intracellular calcium among other cAMP mediated processes. The D2 class of receptors produce the opposite effect, as they are Gαi coupled receptors, and block the activity of adenylyl cyclase. cAMP mediated protein kinase A activity also results in the phosphorylation of DARPP-32, an inhibitor of protein phosphatase 1. Sustained D1 receptor activity is kept in check by Cyclin-dependent kinase 5. Dopamine receptor activation of Ca2+/calmodulin-dependent protein kinase II can be cAMP dependent or independent.[18]
The cAMP mediated pathway results in amplification of PKA phosphorylation activity, which is normally kept in equilibrium by PP1. The DARPP-32 mediated PP1 inhibition amplifies PKA phosphorylation of AMPA, NMDA, and inward rectifying potassium channels, increasing AMPA and NMDA currents while decreasing potassium conductance.[7]
cAMP independent
D1 receptor agonism and D2 receptor blockade also increases mRNA translation by phosphorylating ribosomal protein s6, resulting in activation of mTOR. The behavioral implications are unknown. Dopamine receptors may also regulate ion channels and BDNF independent of cAMP, possibly through direct interactions. There is evidence that D1 receptor agonism regulates phospholipase C independent of cAMP, however implications and mechanisms remain poorly understood. D2 receptor signaling may mediate protein kinase B, arrestin beta 2, and GSK-3 activity, and inhibition of these proteins results in stunting of the hyperlocomotion in amphetamine treated rats. Dopamine receptors can also transactivate Receptor tyrosine kinases.[19]
Beta Arrestin recruitment is mediated by G-protein kinases that phosphorylate and inactivate dopamine receptors after stimulation. While beta arrestin plays a role in receptor desensitization, it may also be critical in mediating downstream effects of dopamine receptors. Beta arrestin has been shown to form complexes with MAP kinase, leading to activation of extracellular signal-regulated kinases. Furthermore, this pathway has been demonstrated to be involved in the locomotor response mediated by dopamine receptor D1. Dopamine receptor D2 stimulation results in the formation of an Akt/Beta-arrestin/PP2A protein complex that inhibits Akt through PP2A phosphorylation, therefore disinhibiting GSK-3.[20]
Role in the central nervous system
Dopamine receptors control neural signaling that modulates many important behaviors, such as spatial working memory.[21] Dopamine also plays an important role in the reward system, incentive salience, cognition, prolactin release, emesis and motor function.[22]
Non-CNS dopamine receptors
Cardio-pulmonary system
In humans, the pulmonary artery expresses D1, D2, D4, and D5 and receptor subtypes, which may account for vasodilatory effects of dopamine in the blood.[23] Such receptor subtypes have also been discovered in the epicardium, myocardium, and endocardium of the heart.[24] In rats, D1-like receptors are present on the smooth muscle of the blood vessels in most major organs.[25]
D4 receptors have been identified in the atria of rat and human hearts.[26] Dopamine increases myocardial contractility and cardiac output, without changing heart rate, by signaling through dopamine receptors.[5]
Renal system
Dopamine receptors are present along the nephron in the kidney, with proximal tubule epithelial cells showing the highest density.[25] In rats, D1-like receptors are present on the juxtaglomerular apparatus and on renal tubules, while D2-like receptors are present on the glomeruli, zona glomerulosa cells of the adrenal cortex, renal tubules, and postganglionic sympathetic nerve terminals.[25] Dopamine signaling affects diuresis and natriuresis.[5]
In disease
Dysfunction of dopaminergic neurotransmission in the CNS has been implicated in a variety of neuropsychiatric disorders, including social phobia,[27] Tourette's syndrome,[28] Parkinson's disease,[29] schizophrenia,[28] neuroleptic malignant syndrome,[30] attention-deficit hyperactivity disorder (ADHD),[31] and drug and alcohol dependence.[28][32]
Attention-deficit hyperactivity disorder
Dopamine receptors have been recognized as important components in the mechanism of ADHD for many years. Drugs used to treat ADHD, including methylphenidate and amphetamine, have significant effects on neuronal dopamine signaling. Studies of gene association have implicated several genes within dopamine signaling pathways; in particular, the D4.7 variant of D4 has been consistently shown to be more frequent in ADHD patients.[33] ADHD patients with the 4.7 allele also tend to have better cognitive performance and long-term outcomes compared to ADHD patients without the 4.7 allele, suggesting that the allele is associated with a more benign form of ADHD.[33]
The D4.7 allele has suppressed gene expression compared to other variants.[34]
Addictive drugs
Dopamine is the primary neurotransmitter involved in the reward pathway in the brain. Thus, drugs that increase dopamine signaling may produce euphoric effects. Many recreational drugs, such as cocaine and substituted amphetamines, inhibit the dopamine transporter (DAT), the protein responsible for removing dopamine from the neural synapse. When DAT activity is blocked, the synapse floods with dopamine and increases dopaminergic signaling. When this occurs, particularly in the nucleus accumbens,[35] increased D1[32] and decreased D2[35] receptor signaling mediates the "rewarding" stimulus of drug intake.[35]
Pathological gambling
Pathological gambling is classified as a mental health disorder that has been linked to obsessive-compulsive spectrum disorder and behavioral addiction. Dopamine has been associated with reward and reinforcement in relation to behaviors and drug addiction.[36] The role between dopamine and pathological gambling may be a link between cerebrospinal fluid measures of dopamine and dopamine metabolites in pathological gambling.[37] Molecular genetic study shows that pathological gambling is associated with the TaqA1 allele of the Dopamine Receptor D2 (DRD2) dopamine receptor. Furthermore, TaqA1 allele is associated with other reward and reinforcement disorders, such as substance abuse and other psychiatric disorders. Reviews of these studies suggest that pathological gambling and dopamine are linked; however, the studies that succeed in controlling for race or ethnicity, and obtain DSM-IV diagnoses do not show a relationship between TaqA1 allelic frequencies and the diagnostic of pathological gambling.[36]
Schizophrenia
While there is evidence that the dopamine system is involved in schizophrenia, the theory that hyperactive dopaminergic signal transduction induces the disease is controversial. Psychostimulants, such as amphetamine and cocaine, indirectly increase dopamine signaling; large doses and prolonged use can induce symptoms that resemble schizophrenia. Additionally, many antipsychotic drugs target dopamine receptors, especially D2 receptors.
Genetic hypertension
Dopamine receptor mutations can cause genetic hypertension in humans.[38] This can occur in animal models and humans with defective dopamine receptor activity, particularly D1.[25]
Parkinson's disease
Parkinson's disease is associated with the degeneration of dopamine and other neurodegenerative events.[36] Parkinson's disease patients are treated with drugs help dopamine function and neurotransmission.[39] Research shows that Parkinson's disease is linked to the class of dopamine agonists instead of specific agents. Reviews touch upon the need to control and regulate dopamine doses for Parkinson's patients who may be predisposed to abusing drugs or not being able to tolerate high doses.[40]
Dopamine regulation
Dopamine receptors are typically stable, however sharp (and sometimes prolonged) increases or decreases in dopamine levels can downregulate (reduce the numbers of) or upregulate (increase the numbers of) dopamine receptors.[41]
Haloperidol, and some other antipsychotics, have been shown to increase the binding capacity of the D2 receptor when used over long periods of time (i.e. increasing the number of such receptors).[42] Haloperidol increased the number of binding sites by 98% above baseline in the worst cases, and yielded significant dyskinesia side effects.
Addictive stimuli have variable effects on dopamine receptors, depending on the particular stimulus.[43] According to one study,[44] cocaine, heroin, amphetamine, alcohol, and nicotine cause decreases in D2 receptor quantity. A similar association has been linked to food addiction, with a low availability of dopamine receptors present in people with greater food intake.[45][46] A recent news article[47] summarized a U.S. DOE Brookhaven National Laboratory study showing that increasing dopamine receptors with genetic therapy temporarily decreased cocaine consumption by up to 75%. The treatment was effective for 6 days. Cocaine upregulates D3 receptors in the nucleus accumbens, possibly contributing to drug seeking behavior.[48]
Certain stimulants will enhance cognition in the general population (e.g., direct or indirect mesocortical DRD1 agonists as a class), but only when used at low (therapeutic) concentrations.[49][50][51] Relatively high doses of dopaminergic stimulants will result in cognitive deficits.[50][51]
See also
- D2 short (presynaptic)
- Category:Dopamine agonists
- Category:Dopamine antagonists
References
- Rondou P, Haegeman G, Van Craenenbroeck K (June 2010). "The dopamine D4 receptor: biochemical and signalling properties". Cellular and Molecular Life Sciences. 67 (12): 1971–86. doi:10.1007/s00018-010-0293-y. PMID 20165900. S2CID 21432517.
- Girault JA, Greengard P (2004). "The neurobiology of dopamine signaling". Arch. Neurol. 61 (5): 641–4. doi:10.1001/archneur.61.5.641. PMID 15148138.
- Cools AR, Van Rossum JM (1976). "Excitation-mediating and inhibition-mediating dopamine-receptors: a new concept towards a better understanding of electrophysiological, biochemical, pharmacological, functional and clinical data". Psychopharmacologia. 45 (3): 243–254. doi:10.1007/bf00421135. PMID 175391. S2CID 40366909.
- Ellenbroek BA, Homberg J, Verheij M, Spooren W, van den Bos R, Martens G (2014). "Alexander Rudolf Cools (1942-2013)". Psychopharmacology. 231 (11): 2219–2222. doi:10.1007/s00213-014-3583-5. PMID 24770629.
- Contreras F, Fouillioux C, Bolívar A, Simonovis N, Hernández-Hernández R, Armas-Hernandez MJ, Velasco M (2002). "Dopamine, hypertension and obesity". J Hum Hypertens. 16 Suppl 1: S13–7. doi:10.1038/sj.jhh.1001334. PMID 11986886.
- Hurley MJ, Jenner P (2006). "What has been learnt from study of dopamine receptors in Parkinson's disease?". Pharmacol. Ther. 111 (3): 715–28. doi:10.1016/j.pharmthera.2005.12.001. PMID 16458973.
- Neve KA, Seamans JK, Trantham-Davidson H (August 2004). "Dopamine receptor signaling". Journal of Receptor and Signal Transduction Research. 24 (3): 165–205. doi:10.1081/RRS-200029981. PMID 15521361. S2CID 12407397.
- Neves SR, Ram PT, Iyengar R (2002). "G protein pathways". Science. 296 (5573): 1636–9. Bibcode:2002Sci...296.1636N. doi:10.1126/science.1071550. PMID 12040175. S2CID 20136388.
- "Introduction to Neuroscience".
- Suzuki M, Hurd YL, Sokoloff P, Schwartz JC, Sedvall G (1998). "D3 dopamine receptor mRNA is widely expressed in the human brain". Brain Res. 779 (1–2): 58–74. doi:10.1016/S0006-8993(97)01078-0. PMID 9473588. S2CID 46096849.
- NCBI Database
- Manor I, Tyano S, Eisenberg J, Bachner-Melman R, Kotler M, Ebstein RP (2002). "The short DRD4 repeats confer risk to attention deficit hyperactivity disorder in a family-based design and impair performance on a continuous performance test (TOVA)". Mol. Psychiatry. 7 (7): 790–4. doi:10.1038/sj.mp.4001078. PMID 12192625.
- Langley K, Marshall L, van den Bree M, Thomas H, Owen M, O'Donovan M, Thapar A (2004). "Association of the dopamine D4 receptor gene 7-repeat allele with neuropsychological test performance of children with ADHD". Am J Psychiatry. 161 (1): 133–8. doi:10.1176/appi.ajp.161.1.133. PMID 14702261. S2CID 25892078.
- Kustanovich V, Ishii J, Crawford L, Yang M, McGough JJ, McCracken JT, Smalley SL, Nelson SF (2004). "Transmission disequilibrium testing of dopamine-related candidate gene polymorphisms in ADHD: confirmation of association of ADHD with DRD4 and DRD5". Mol. Psychiatry. 9 (7): 711–7. doi:10.1038/sj.mp.4001466. PMID 14699430.
- Beaulieu JM, Espinoza S, Gainetdinov RR (2015). "Dopamine receptors – IUPHAR Review 13". Br. J. Pharmacol. 172 (1): 1–23. doi:10.1111/bph.12906. PMC 4280963. PMID 25671228.
- Borroto-Escuela DO, Brito I, Romero-Fernandez W, et al. (May 2014). "The G protein-coupled receptor heterodimer network (GPCR-HetNet) and its hub components". Int J Mol Sci. 15 (5): 8570–90. doi:10.3390/ijms15058570. PMC 4057749. PMID 24830558.
- Agnati LF, Guidolin D, Cervetto C, Borroto-Escuela DO, Fuxe K (January 2016). "Role of iso-receptors in receptor-receptor interactions with a focus on dopamine iso-receptor complexes". Rev Neurosci. 27 (1): 1–25. doi:10.1515/revneuro-2015-0024. PMID 26418645.
- Beaulieu JM, Espinoza S, Gainetdinov RR (January 2015). "Dopamine receptors – IUPHAR Review 13". British Journal of Pharmacology. 172 (1): 1–23. doi:10.1111/bph.12906. PMC 4280963. PMID 25671228.
- name="receptor mechanism"
- Del'guidice T, Lemasson M, Beaulieu JM (2011). "Role of Beta-arrestin 2 downstream of dopamine receptors in the Basal Ganglia". Frontiers in Neuroanatomy. 5: 58. doi:10.3389/fnana.2011.00058. PMC 3167352. PMID 21922001.
- Williams GV, Castner SA (2006). "Under the curve: critical issues for elucidating D1 receptor function in working memory". Neuroscience. 139 (1): 263–76. doi:10.1016/j.neuroscience.2005.09.028. PMID 16310964. S2CID 20906770.
- Webster R (2001). Neurotransmitters, drugs and brain function (Repr. ed.). Chichester: Wiley. p. 137. ISBN 978-0-471-97819-0.
- Ricci A, Mignini F, Tomassoni D, Amenta F (2006). "Dopamine receptor subtypes in the human pulmonary arterial tree". Auton Autacoid Pharmacol. 26 (4): 361–9. doi:10.1111/j.1474-8673.2006.00376.x. PMID 16968475.
- Cavallotti C, Massimo M, Paolo B, Maurizio S, Fiorenzo M (2010). "Dopamine receptor subtypes in the native human heart". Heart and Vessels. 25 (5): 432–7. doi:10.1007/s00380-009-1224-4. PMID 20676967. S2CID 36507640.
- Hussain T, Lokhandwala MF (2003). "Renal dopamine receptors and hypertension". Exp. Biol. Med. (Maywood). 228 (2): 134–42. doi:10.1177/153537020322800202. PMID 12563019. S2CID 10896819.
- Ricci A, Bronzetti E, Fedele F, Ferrante F, Zaccheo D, Amenta F (1998). "Pharmacological characterization and autoradiographic localization of a putative dopamine D4 receptor in the heart". J Auton Pharmacol. 18 (2): 115–21. doi:10.1046/j.1365-2680.1998.1820115.x. PMID 9730266.
- Schneier FR, Liebowitz MR, Abi-Dargham A, Zea-Ponce Y, Lin SH, Laruelle M (2000). "Low dopamine D(2) receptor binding potential in social phobia". Am J Psychiatry. 157 (3): 457–459. doi:10.1176/appi.ajp.157.3.457. PMID 10698826.
- Kienast T, Heinz A (2006). "Dopamine and the diseased brain". CNS Neurol Disord Drug Targets. 5 (1): 109–31. doi:10.2174/187152706784111560. PMID 16613557.
- Fuxe K, Manger P, Genedani S, Agnati L (2006). "The nigrostriatal DA pathway and Parkinson's disease". J. Neural Transm. Suppl. Journal of Neural Transmission. Supplementa. 70 (70): 71–83. doi:10.1007/978-3-211-45295-0_13. ISBN 978-3-211-28927-3. PMID 17017512.
- Mihara K, et al. (2003). "Relationship between functional dopamine D2 and D3 receptors gene polymorphisms and neuroleptic malignant syndrome". Am. J. Med. Genet. B Neuropsychiatr. Genet. 117B (1): 57–60. doi:10.1002/ajmg.b.10025. PMID 12555236. S2CID 44866985.
- Faraone SV, Khan SA (2006). "Candidate gene studies of attention-deficit/hyperactivity disorder". J Clin Psychiatry. 67 Suppl 8: 13–20. PMID 16961425.
- Hummel M, Unterwald EM (2002). "D1 dopamine receptor: a putative neurochemical and behavioral link to cocaine action". J. Cell. Physiol. 191 (1): 17–27. doi:10.1002/jcp.10078. PMID 11920678. S2CID 40444893.
- Gornick MC, Addington A, Shaw P, Bobb AJ, Sharp W, Greenstein D, Arepalli S, Castellanos FX, Rapoport JL (2007). "Association of the dopamine receptor D4 (DRD4) gene 7-repeat allele with children with attention-deficit/hyperactivity disorder (ADHD): an update". Am. J. Med. Genet. B Neuropsychiatr. Genet. 144B (3): 379–82. doi:10.1002/ajmg.b.30460. PMID 17171657. S2CID 25065281.
- Schoots O, Van Tol HH (2003). "The human dopamine D4 receptor repeat sequences modulate expression". Pharmacogenomics J. 3 (6): 343–8. doi:10.1038/sj.tpj.6500208. PMID 14581929.
- Di Chiara G, Bassareo V, Fenu S, De Luca MA, Spina L, Cadoni C, Acquas E, Carboni E, Valentini V, Lecca D (2004). "Dopamine and drug addiction: the nucleus accumbens shell connection". Neuropharmacology. 47 Suppl 1: 227–41. doi:10.1016/j.neuropharm.2004.06.032. PMID 15464140. S2CID 25983940.
- Potenza MN (October 2008). "Review. The neurobiology of pathological gambling and drug addiction: an overview and new findings". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 363 (1507): 3181–9. doi:10.1098/rstb.2008.0100. PMC 2607329. PMID 18640909.
- Leibenluft E (October 1999). "Gender differences in major depressive disorder and bipolar disorder". CNS Spectrums. 4 (10): 25–33. doi:10.1017/S1092852900012335. PMID 18438310.
- Jose PA, Eisner GM, Felder RA (2003). "Regulation of blood pressure by dopamine receptors". Nephron Physiol. 95 (2): 19–27. doi:10.1159/000073676. PMID 14610323. S2CID 28595227.
- Lang AE, Obeso JA (May 2004). "Challenges in Parkinson's disease: restoration of the nigrostriatal dopamine system is not enough". The Lancet. Neurology. 3 (5): 309–16. doi:10.1016/S1474-4422(04)00740-9. PMID 15099546. S2CID 6551470.
- Nestler EJ (1 January 2004). "Molecular mechanisms of drug addiction". Neuropharmacology. 47 Suppl 1: 24–32. doi:10.1016/j.neuropharm.2004.06.031. PMID 15464123. S2CID 11266116.
- Scheler, G. (2004). "Regulation of neuromodulator receptor efficacy--implications for whole-neuron and synaptic plasticity". Prog. Neurobiol. 72 (6): 399–415. arXiv:q-bio/0401039. doi:10.1016/j.pneurobio.2004.03.008. PMID 15177784. S2CID 9353254.
- Silvestri S, et al. (2000). "Increased dopamine D2 receptor binding after long-term treatment with antipsychotics in humans: a clinical PET study". Psychopharmacology. 152 (2): 174–80. doi:10.1007/s002130000532. PMID 11057521. S2CID 20804595.
- Olsen CM (December 2011). "Natural rewards, neuroplasticity, and non-drug addictions". Neuropharmacology. 61 (7): 1109–22. doi:10.1016/j.neuropharm.2011.03.010. PMC 3139704. PMID 21459101.
Cross-sensitization is also bidirectional, as a history of amphetamine administration facilitates sexual behavior and enhances the associated increase in NAc DA ... As described for food reward, sexual experience can also lead to activation of plasticity-related signaling cascades. The transcription factor delta FosB is increased in the NAc, PFC, dorsal striatum, and VTA following repeated sexual behavior (Wallace et al., 2008; Pitchers et al., 2010b). This natural increase in delta FosB or viral overexpression of delta FosB within the NAc modulates sexual performance, and NAc blockade of delta FosB attenuates this behavior (Hedges et al, 2009; Pitchers et al., 2010b). Further, viral overexpression of delta FosB enhances the conditioned place preference for an environment paired with sexual experience (Hedges et al., 2009). ... In some people, there is a transition from “normal” to compulsive engagement in natural rewards (such as food or sex), a condition that some have termed behavioral or non-drug addictions (Holden, 2001; Grant et al., 2006a). ... In humans, the role of dopamine signaling in incentive-sensitization processes has recently been highlighted by the observation of a dopamine dysregulation syndrome in some patients taking dopaminergic drugs. This syndrome is characterized by a medication-induced increase in (or compulsive) engagement in non-drug rewards such as gambling, shopping, or sex (Evans et al, 2006; Aiken, 2007; Lader, 2008)."
Table 1" - Fehr C, et al. (April 2008). "Association of low striatal dopamine d2 receptor availability with nicotine dependence similar to that seen with other drugs of abuse". The American Journal of Psychiatry. 165 (4): 507–14. doi:10.1176/appi.ajp.2007.07020352. PMID 18316420.
- Park P (9 August 2007). "Food Addiction: From Drugs to Donuts, Brain Activity May be the Key".
- Johnson PM, Kenny PJ (May 2010). "Dopamine D2 receptors in addiction-like reward dysfunction and compulsive eating in obese rats". Nature Neuroscience. 13 (5): 635–41. doi:10.1038/nn.2519. PMC 2947358. PMID 20348917.
- "Gene Therapy For Addiction: Flooding Brain With 'Pleasure Chemical' Receptors Works On Cocaine, As On Alcohol". 18 April 2008.
- Staley JK, Mash DC (October 1996). "Adaptive increase in D3 dopamine receptors in the brain reward circuits of human cocaine fatalities". The Journal of Neuroscience. 16 (19): 6100–6. doi:10.1523/JNEUROSCI.16-19-06100.1996. PMC 6579196. PMID 8815892.
- Ilieva IP, Hook CJ, Farah MJ (January 2015). "Prescription Stimulants' Effects on Healthy Inhibitory Control, Working Memory, and Episodic Memory: A Meta-analysis". J. Cogn. Neurosci. 27 (6): 1069–1089. doi:10.1162/jocn_a_00776. PMID 25591060. S2CID 15788121.
The present meta-analysis was conducted to estimate the magnitude of the effects of methylphenidate and amphetamine on cognitive functions central to academic and occupational functioning, including inhibitory control, working memory, short-term episodic memory, and delayed episodic memory. In addition, we examined the evidence for publication bias. Forty-eight studies (total of 1,409 participants) were included in the analyses. We found evidence for small but significant stimulant enhancement effects on inhibitory control and short-term episodic memory. Small effects on working memory reached significance, based on one of our two analytical approaches. Effects on delayed episodic memory were medium in size. However, because the effects on long-term and working memory were qualified by evidence for publication bias, we conclude that the effect of amphetamine and methylphenidate on the examined facets of healthy cognition is probably modest overall. In some situations, a small advantage may be valuable, although it is also possible that healthy users resort to stimulants to enhance their energy and motivation more than their cognition. ... Earlier research has failed to distinguish whether stimulants’ effects are small or whether they are nonexistent (Ilieva et al., 2013; Smith & Farah, 2011). The present findings supported generally small effects of amphetamine and methylphenidate on executive function and memory. Specifically, in a set of experiments limited to high-quality designs, we found significant enhancement of several cognitive abilities. ...
The results of this meta-analysis cannot address the important issues of individual differences in stimulant effects or the role of motivational enhancement in helping perform academic or occupational tasks. However, they do confirm the reality of cognitive enhancing effects for normal healthy adults in general, while also indicating that these effects are modest in size. - Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 13: Higher Cognitive Function and Behavioral Control". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. 318. ISBN 9780071481274.
Mild dopaminergic stimulation of the prefrontal cortex enhances working memory. ...
Therapeutic (relatively low) doses of psychostimulants, such as methylphenidate and amphetamine, improve performance on working memory tasks both in normal subjects and those with ADHD. Positron emission tomography (PET) demonstrates that methylphenidate decreases regional cerebral blood flow in the doroslateral prefrontal cortex and posterior parietal cortex while improving performance of a spatial working memory task. This suggests that cortical networks that normally process spatial working memory become more efficient in response to the drug. ... [It] is now believed that dopamine and norepinephrine, but not serotonin, produce the beneficial effects of stimulants on working memory. At abused (relatively high) doses, stimulants can interfere with working memory and cognitive control ... stimulants act not only on working memory function, but also on general levels of arousal and, within the nucleus accumbens, improve the saliency of tasks. Thus, stimulants improve performance on effortful but tedious tasks ... through indirect stimulation of dopamine and norepinephrine receptors. - Wood S, Sage JR, Shuman T, Anagnostaras SG (January 2014). "Psychostimulants and cognition: a continuum of behavioral and cognitive activation". Pharmacol. Rev. 66 (1): 193–221. doi:10.1124/pr.112.007054. PMC 3880463. PMID 24344115.
External links
- "Dopamine Receptors". IUPHAR Database of Receptors and Ion Channels. International Union of Basic and Clinical Pharmacology.
- Zimmerberg, B., "Dopamine receptors: A representative family of metabotropic receptors, Multimedia Neuroscience Education Project (2002)
- Scholarpedia article on Dopamine anatomy