Promethazine
Promethazine is a first-generation antihistamine used to treat allergies, difficulty sleeping, and nausea.[4] It may also help with some symptoms associated with the common cold[4] and may also be used for sedating people who are agitated or anxious.[5][6] Promethazine is available by mouth in syrup or tablet dosage forms, as a rectal suppository, or by injection into a muscle.[4]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Phenergan, many others[1] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682284 |
| Pregnancy category |
|
| Routes of administration | By mouth, rectal, IV, IM, topical |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 88% absorbed but after first-pass metabolism reduced to 25% absolute bioavailability[2] |
| Protein binding | 93% |
| Metabolism | Liver glucuronidation and sulfoxidation |
| Elimination half-life | 10–19 hours[2][3] |
| Excretion | Kidney and biliary |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.445 |
| Chemical and physical data | |
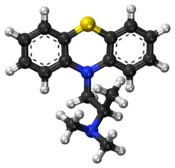
| Formula | C17H20N2S |
| Molar mass | 284.42 g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| |
| |
| (verify) | |
Common side effects of promethazine include confusion and sleepiness;[4] consumption of alcohol or other sedatives can make these symptoms worse.[4] It is unclear if use of promethazine during pregnancy or breastfeeding is safe for the baby.[4][5] Use of promethazine is not recommended in those less than two years old, due to potentially negative effects on breathing.[4] Use of promethazine by injection into a vein is not recommended, due to potential skin damage.[4] Promethazine is in the phenothiazine family of medications.[4]
Promethazine was made in the 1940s by a team of scientists from Rhône-Poulenc laboratories.[7] It was approved for medical use in the United States in 1951.[4] It is a generic medication and is available under many brand names globally.[1] In 2017, promethazine was the 147th-most commonly prescribed medication in the United States, with more than four million prescriptions.[8][9]
Medical uses
Promethazine has a variety of medical uses, including:
- Sedation[10]
- Nausea and vomiting association with anesthesia or chemotherapy. It is commonly used postoperatively as an antiemetic. The antiemetic activity increases with increased dosing; however, side effects also increase, which often limits maximal dosing.[10]
- For moderate to severe morning sickness and hyperemesis gravidarum: In the UK, promethazine is drug of first choice, being preferred as an older drug with which there is a greater experience of use in pregnancy (second in line being metoclopramide or prochlorperazine).[11][10]
- For allergies such as hay fever and together with other medications in anaphylaxis[4]
- To aid with symptoms of the common cold[4]
- Motion sickness[4]
- Hemolytic disease of the newborn[4]
- Anxiety before surgery[4]
Side effects
Some documented side effects include:
- Tardive dyskinesia, pseuodoparkinsonism, acute dystonia (effects due to dopamine D2 receptor antagonism)[10]
- Confusion in the elderly[10]
- Drowsiness, dizziness, fatigue, more rarely vertigo
- Known to have effects on serotonin and dopamine receptors.[12]
- Dry mouth[10]
- Nausea[13]
- Respiratory depression in patients under age of two and in those with severely compromised pulmonary function
- Blurred vision, xerostomia, dry nasal passages, dilated pupils, constipation, and urinary retention. (due to cholinergic effects)[10]
- Chest discomfort/pressure (In children less than 2 years old)[10]
- Akathisia[14]
Less frequent:
- Cardiovascular side effects to include arrhythmias and hypotension[10]
- Neuroleptic malignant syndrome[10]
- Liver damage and cholestatic jaundice[10]
- Bone marrow suppression, potentially resulting in agranulocytosis, thrombocytopenia, and leukopenia[10]
- Depression of the thermoregulatory mechanism resulting in hypothermia/hyperthermia[10]
Rare side effects include:
Because of potential for more severe side effects, this drug is on the list to avoid in the elderly.[15] In many countries (including the US and UK), promethazine is contraindicated in children less than two years of age, and strongly cautioned against in children between two and six, due to problems with respiratory depression and sleep apnea.[16]
Promethazine is listed as one of the drugs of highest anticholinergic activity in a study of anticholinergenic burden, including long-term cognitive impairment.[17]
Pharmacology
Promethazine, a phenothiazine derivative, is structurally different from the neuroleptic phenothiazines, with similar but different effects.[2] It acts primarily as a strong antagonist of the H1 receptor (antihistamine) and a moderate mACh receptor antagonist (anticholinergic),[2] and also has weak to moderate affinity for the 5-HT2A,[18] 5-HT2C,[18] D2,[19][20] and α1-adrenergic receptors,[21] where it acts as an antagonist at all sites, as well.
Another notable use of promethazine is as a local anesthetic, by blockade of sodium channels.[21]
Chemistry
Solid promethazine hydrochloride is a white to faint-yellow, practically odorless, crystalline powder. Slow oxidation may occur upon prolonged exposure to air, usually causing blue discoloration. Its hydrochloride salt is freely soluble in water and somewhat soluble in alcohol. Promethazine is a chiral compound, occurring as a mixture of enantiomers.[22]
History
Promethazine was first synthesized by a group at Rhone-Poulenc (which later became part of Sanofi) led by Paul Charpentier in the early 1940s.[23] The team was seeking to improve on diphenhydramine; the same line on medical chemistry led to the creation of chlorpromazine.[24]
Society and culture
As of July 2017 it was marketed under many brand names worldwide: Allersoothe, Antiallersin, Anvomin, Atosil, Avomine, Closin N, Codopalm, Diphergan, Farganesse, Fenazil, Fenergan, Fenezal, Frinova, Hiberna, Histabil, Histaloc, Histantil, Histazin, Histazine, Histerzin, Lenazine, Lergigan, Nufapreg, Otosil, Pamergan, Pharmaniaga, Phenadoz, Phenerex, Phenergan, Phénergan, Pipolphen, Polfergan, Proazamine, Progene, Prohist, Promet, Prometal, Prometazin, Prometazina, Promethazin, Prométhazine, Promethazinum, Promethegan, Promezin, Proneurin, Prothazin, Prothiazine, Prozin, Pyrethia, Quitazine, Reactifargan, Receptozine, Romergan, Sominex, Sylomet, Xepagan, Zinmet, and Zoralix.[1]
It is also marketed in many combination drug formulations:
- with carbocisteine as Actithiol Antihistaminico, Mucoease, Mucoprom, Mucotal Prometazine, and Rhinathiol;
- with paracetamol (acetaminophen) as Algotropyl, Calmkid, Fevril, Phen Plus, and Velpro-P;
- with paracetamol and dextromethorphan as Choligrip na noc, Coldrex Nočná Liečba, Fedril Night Cold and Flu, Night Nurse, and Tachinotte;
- with paracetamol, phenylephrine, and salicylamide as Flukit;
- with dextromethorphan as Axcel Dextrozine and Hosedyl DM;
- with dextromethorphan and ephedrine as Methorsedyl;
- with dextromethorphan and pseudoephedrine as Sedilix-DM;
- with dextromethorphan and phenylephedrine as Sedilix-RX;
- with pholcodine as Codo-Q Junior and Tixylix;
- with pholcodine and ephedrine as Phensedyl Dry Cough Linctus;
- with pholcodine and phenylephedrine as Russedyl Compound Linctus;
- with pholcodine and phenylpropanolamine as Triple 'P';
- with codeine as Kefei and Procodin;
- with codeine and ephedrine as Dhasedyl, Fendyl, and P.E.C.;
- with ephedrine and dextromethorphan as Dhasedyl DM;
- with glutamic acid as Psico-Soma, and Psicosoma;
- with noscapine as Tussisedal; and
- with chlorpromazine and phenobarbital as Vegetamin.[1]
Recreational use
The recreational drug purple drank often contains a combination of promethazine with codeine containing cold medication.[25]
Product liability lawsuit
In 2009, the US Supreme Court ruled on a product liability case involving promethazine. Diana Levine, a woman suffering from a migraine, was administered Wyeth's Phenergan via IV push. The drug was injected improperly, resulting in gangrene and subsequent amputation of her right forearm below the elbow. A state jury awarded her $6 million in punitive damages.
The case was appealed to the Supreme Court on grounds of federal preemption and substantive due process.[26] The Supreme Court upheld the lower courts' rulings, stating that "Wyeth could have unilaterally added a stronger warning about IV-push administration" without acting in opposition to federal law.[27] In effect, this means drug manufacturers can be held liable for injuries if warnings of potential adverse effects, approved by the US Food and Drug Administration (FDA), are deemed insufficient by state courts.
On September 9, 2009, the FDA required a boxed warning be put on promethazine for injection, stating the contraindication for subcutaneous administration. The preferred administrative route is intramuscular, which reduces risk of surrounding muscle and tissue damage.[28]
References
- "Promethazine international brands". Drugs.com. Retrieved 17 July 2017.
- Strenkoski-Nix LC, Ermer J, DeCleene S, Cevallos W, Mayer PR (August 2000). "Pharmacokinetics of promethazine hydrochloride after administration of rectal suppositories and oral syrup to healthy subjects". American Journal of Health-System Pharmacy. 57 (16): 1499–505. doi:10.1093/ajhp/57.16.1499. PMID 10965395.
- Paton DM, Webster DR (1985). "Clinical pharmacokinetics of H1-receptor antagonists (the antihistamines)". Clinical Pharmacokinetics. 10 (6): 477–97. doi:10.2165/00003088-198510060-00002. PMID 2866055. S2CID 33541001.
- "Promethazine Hydrochloride Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Retrieved 24 October 2018.
- British national formulary : BNF 74 (74 ed.). British Medical Association. 2017. p. 276. ISBN 978-0857112989.
- Malamed, Stanley F. (2009). Sedation: A Guide to Patient Management. Elsevier Health Sciences. p. 113. ISBN 978-0323075961.
- Li, Jie Jack (2006). Laughing Gas, Viagra, and Lipitor: The Human Stories behind the Drugs We Use. United Kingdom: Oxford University Press. p. 146. ISBN 9780199885282. Retrieved July 9, 2016.
- "The Top 300 of 2020". ClinCalc. Retrieved 11 April 2020.
- "Promethazine Hydrochloride - Drug Usage Statistics". ClinCalc. Retrieved 11 April 2020.
- Southard BT, Al Khalili Y (2019). "Promethazine". StatPearls. PMID 31335081.
 This article incorporates text available under the CC BY 4.0 license.
This article incorporates text available under the CC BY 4.0 license. - British National Formulary (March 2001). "4.6 Drugs used in nausea and Vertigo - Vomiting of pregnancy". BNF (45 ed.)..
- Schreiner, Nicole, Windham, Samuel, Barker, Andrew. Atypical Neuroleptic Malignant Syndrome: Diagnosis and Proposal for an Expanded Treatment Algorithm: A Case Report. A&A Case Reports. 2017;9(12):339-343. doi:10.1213/XAA.0000000000000610.
- National Institute for Health and Care Excellence
- Cordingley Neurology
- NCQA’s HEDIS Measure: Use of High Risk Medications in the Elderly Archived 2010-02-01 at the Wayback Machine
- Starke P, Weaver J, Chowdhury B (2005). "Boxed warning added to promethazine labeling for pediatric use". N. Engl. J. Med. 352 (5): 2653. doi:10.1056/nejm200506233522522. PMID 15972879.
- Salahudeen MJ; Duffull SB; Nishtala PS; et al. (2015-03-25). "Anticholinergic burden quantified by anticholinergic risk scales and adverse outcomes in older people: a systematic review". BMC Geriatrics. 15 (31): 31. doi:10.1186/s12877-015-0029-9. PMC 4377853. PMID 25879993.
- Fiorella D, Rabin RA, Winter JC (October 1995). "The role of the 5-HT2A and 5-HT2C receptors in the stimulus effects of hallucinogenic drugs. I: Antagonist correlation analysis". Psychopharmacology. 121 (3): 347–56. doi:10.1007/bf02246074. PMID 8584617. S2CID 24420080.
- Seeman P, Watanabe M, Grigoriadis D, et al. (November 1985). "Dopamine D2 receptor binding sites for agonists. A tetrahedral model". Molecular Pharmacology. 28 (5): 391–9. PMID 2932631.
- Burt DR, Creese I, Snyder SH (April 1977). "Antischizophrenic drugs: chronic treatment elevates dopamine receptor binding in brain". Science. 196 (4287): 326–8. Bibcode:1977Sci...196..326B. doi:10.1126/science.847477. PMID 847477.
- Jagadish Prasad, P. (2010). Conceptual Pharmacology. Universities Press. pp. 295, 303, 598. ISBN 978-81-7371-679-9. Retrieved 27 November 2011.
- "RxList: Promethazine Description". 2007-06-21. Archived from the original on 2008-09-11. Retrieved 2008-06-04.
- Ban, TA (2006). "The role of serendipity in drug discovery". Dialogues in Clinical Neuroscience. 8 (3): 335–44. PMC 3181823. PMID 17117615.
- "Paul Charpentier, Henri-Marie Laborit, Simone Courvoisier, Jean Delay, and Pierre Deniker". Science History Institute. August 6, 2015. Retrieved 20 March 2018.
- Agnich, LE; Stogner, JM; Miller, BL; Marcum, CD (September 2013). "Purple drank prevalence and characteristics of misusers of codeine cough syrup mixtures" (PDF). Addictive Behaviors. 38 (9): 2445–9. doi:10.1016/j.addbeh.2013.03.020. PMID 23688907.
- Liptak, Adam (2001-09-18). "Drug Label, Maimed Patient and Crucial Test for Justices". The New York Times. Retrieved 2008-10-31.
- Stout, David (2009-03-04). "Drug Approval Is Not a Shield From Lawsuits, Justices Rule". The New York Times. Retrieved 2009-03-04.
- "Information for Healthcare Professionals: Intravenous Promethazine and Severe Tissue Injury, Including Gangrene". 2013-08-15.