Pharmacology of cyproterone acetate
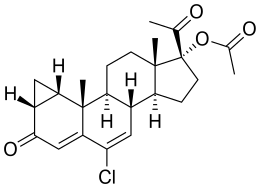
The pharmacology of cyproterone acetate (CPA), concerns the pharmacology (pharmacodynamics, pharmacokinetics, and routes of administration) of the steroidal antiandrogen and progestin medication cyproterone acetate.
 | |
| Clinical data | |
|---|---|
| Routes of administration | By mouth, intramuscular injection |
| Drug class | Steroidal antiandrogen; Progestin; Progestogen; Progestogen ester; Antigonadotropin |
| Pharmacokinetic data | |
| Bioavailability | Oral: 68–100%[1][2] |
| Protein binding | Albumin: 93% Free: 7%[3][4][5][6] |
| Metabolism | Hepatic (CYP3A4)[7][8] |
| Metabolites | • 15β-OH-CPA (major)[1][9] • Cyproterone (minor)[10] • Acetic acid (minor)[10] |
| Elimination half-life | Oral: 1.6–4.3 days[10][11][12] IM: 3–4.3 days[2][10][12] |
| Excretion | Feces: 70%[10] Urine: 30%[10] |
CPA blocks the effects of androgens like testosterone in the body, which it does by preventing them from interacting with their biological target, the androgen receptor (AR), and by reducing their production by the gonads and hence their concentrations in the body.[1][13][14] In addition, it has progesterone-like effects by activating the progesterone receptor (PR).[1][13] By activating the PR, CPA has antigonadotropic effects and can inhibit fertility and suppress sex hormone production in both men and women. CPA can also produce weak and partial cortisol-like effects at very high doses under certain circumstances by activating the glucocorticoid receptor (GR).[1]
CPA can be taken by mouth or by injection into muscle. It has near-complete oral bioavailability, is highly and exclusively bound to albumin in terms of plasma protein binding, is metabolized in the liver by hydroxylation and conjugation, has 15β-hydroxycyproterone acetate (15β-OH-CPA) as a single major active metabolite, has a long elimination half-life of about 2 to 4 days regardless of route of administration, and is excreted in feces primarily and to a lesser extent in urine.
Pharmacodynamics
CPA has antiandrogenic activity,[1][15] progestogenic activity,[1][15] weak partial glucocorticoid activity,[16] weak steroidogenesis inhibitor activity,[17] and agonist activity at the pregnane X receptor.[18][19][20] It has no estrogenic or antimineralocorticoid activity.[1] In terms of potency, CPA is described as a highly potent progestogen, a moderately potent antiandrogen, and a weak glucocorticoid.[21][22][23]
| Progestogen | PR | AR | ER | GR | MR |
|---|---|---|---|---|---|
| Cyproterone acetate | 90 | 6 | 0 | 6 | 8 |
| Notes: Values are percentages (%). Reference ligands (100%) were promegestone for the PR, metribolone for the AR, estradiol for the ER, dexamethasone for the GR, and aldosterone for the MR. Sources: [1] | |||||
| Antiandrogen | AR | PR | ER | GR | MR |
|---|---|---|---|---|---|
| Cyproterone acetate | 8–10 | 60 | <0.1 | 5 | 1 |
| Chlormadinone acetate | 5 | 175 | <0.1 | 38 | 1 |
| Megestrol acetate | 5 | 152 | <0.1 | 50 | 3 |
| Spironolactone | 7 | 0.4a | <0.1 | 2a | 182 |
| Trimethyltrienolone | 3.6 | <1 | <1 | <1 | <1 |
| Inocoterone | 0.8 | <0.1 | <0.1 | <0.1 | <0.1 |
| Inocoterone acetate | <0.1 | <0.1 | <0.1 | <0.1 | <0.1 |
| Flutamide | <0.1 | <0.1 | <0.1 | <0.1 | <0.1 |
| Hydroxyflutamide | 0.5–0.8 | <0.1 | <0.1 | <0.1 | <0.1 |
| Nilutamide | 0.5–0.8 | <0.1 | <0.1 | <0.1 | <0.1 |
| Bicalutamide | 1.8 | <0.1 | <0.1 | <0.1 | <0.1 |
| Notes: (1): Reference ligands (100%) were testosterone for the AR, progesterone for the PR, estradiol for the ER, dexamethasone for the GR, and aldosterone for the MR. (2): Tissues were rat prostate (AR), rabbit uterus (PR), mouse uterus (ER), rat thymus (GR), and rat kidney (MR). (3): Incubation times (0°C) were 24 hours (AR, a), 2 hours (PR, ER), 4 hours (GR), and 1 hour (MR). (4): Assay methods were different for bicalutamide for receptors besides the AR. Sources: See template. | |||||
| Compound | Form | Dose for specific uses (mg)[lower-alpha 3] | DOA[lower-alpha 4] | |||
|---|---|---|---|---|---|---|
| TFD[lower-alpha 5] | POICD[lower-alpha 6] | CICD[lower-alpha 7] | ||||
| Algestone acetophenide | Oil soln. | - | – | 75–150 | 14–32 d | |
| Gestonorone caproate | Oil soln. | 25–50 | – | – | 8–13 d | |
| Hydroxyprogest. acetate[lower-alpha 8] | Aq. susp. | 350 | – | – | 9–16 d | |
| Hydroxyprogest. caproate | Oil soln. | 250–500[lower-alpha 9] | – | 250–500 | 5–21 d | |
| Medroxyprog. acetate | Aq. susp. | 50–100 | 150 | 25 | 14–50+ d | |
| Megestrol acetate | Aq. susp. | - | – | 25 | >14 d | |
| Norethisterone enanthate | Oil soln. | 100–200 | 200 | 50 | 11–52 d | |
| Progesterone | Oil soln. | 200[lower-alpha 9] | – | – | 2–6 d | |
| Aq. soln. | ? | – | – | 1–2 d | ||
| Aq. susp. | 50–200 | – | – | 7–14 d | ||
|
Notes and sources:
| ||||||
Antiandrogenic activity
| Compound | RBA[lower-alpha 2] |
|---|---|
| Metribolone | 100 |
| Dihydrotestosterone | 85 |
| Cyproterone acetate | 7.8 |
| Bicalutamide | 1.4 |
| Nilutamide | 0.9 |
| Hydroxyflutamide | 0.57 |
| Flutamide | <0.0057 |
Notes:
| |
| Antiandrogen | Relative potency |
|---|---|
| Bicalutamide | 4.3 |
| Hydroxyflutamide | 3.5 |
| Flutamide | 3.3 |
| Cyproterone acetate | 1.0 |
| Zanoterone | 0.4 |
| Description: Relative potencies of orally administered antiandrogens in antagonizing 0.8 to 1.0 mg/kg s.c. testosterone propionate-induced ventral prostate weight increase in castrated immature male rats. Sources: See template. | |
CPA is a potent competitive antagonist of the androgen receptor (AR), the biological target of androgens such as testosterone and dihydrotestosterone (DHT).[15] It was at one time the most potent known AR antagonist of the steroidal antiandrogens,[45] out of hundreds of other compounds.[46] CPA has the highest antiandrogenic activity of any other clinically used progestin.[47][48] It directly blocks endogenous androgens like testosterone and DHT from binding to and activating the AR, and thus prevents them from exerting their androgenic effects, such as masculinization and prostate gland growth, in the body.[49][47]
A comparative study of binding inhibition to the AR in rat prostate cytosol AR found IC50 values of 3 nM for DHT, 24 nM for cyproterone acetate, and 67 nM for spironolactone.[50]
| Compound | AR RBA (%) | AR Ki (nM) |
|---|---|---|
| Metribolone | 100 | 1.18 |
| Dihydrotestosterone | 136 | 0.87 |
| Testosterone | 117 | 1.01 |
| Spironolactone | 67.0 | 1.76 |
| Trimethyltrienolone | 14.8 | 8.0 |
| Megestrol acetate | 13.6 | 8.7 |
| Cyproterone acetate | 12.5 | 9.5 |
| Progesterone | 6.6 | 18 |
| Estradiol | 4.9 | 24 |
| Androstenedione | 2.0 | 58 |
| Canrenone | 0.84 | 140 |
| Flutamide | 0.079 | 1200 |
| Cimetidine | 0.00084 | 140,000 |
| Notes: (1) Human skin fibroblasts used for assays. (2) Situation in vivo is different for flutamide and spironolactone due biotransformation. (3) Conflicting findings for spironolactone. Sources: Main: [21][51] Related: [52][53][54] | ||
Antiandrogenic efficacy and potency
The antiandrogenic activity of CPA is dose-dependent.[47][55] Although CPA is a potent antiandrogen, relatively high doses of CPA are nonetheless required for clinically important AR antagonism.[56][55][21] The clinical antiandrogenic efficacy of birth control pills containing CPA, which have only low doses of CPA in them (2 mg/day), often can't be distinguished from that of birth control pills containing other progestins.[56] It is likely that the antiandrogenic effects of CPA-containing birth control pills are due mostly to the ethinylestradiol component and/or suppression of androgen levels, rather than the antiandrogenic activity of the small doses of CPA present in them.[57][21][58][59][55]
CPA has been found to decrease inflammatory acne lesions in males by about 15% at 5 mg/day, by 45% at 25 mg/day, and by 73% at 100 mg/day.[60] A dosage of 100 mg/day CPA can achieve a 65 to 70% reduction in sebum excretion rate in males within 4 weeks of treatment, but doses of 10 mg/day CPA or less are said to have a negligible effect.[57][58] On the basis of these findings, it has estimated that the threshold dosage of CPA to reduce sebum production may be 5 mg/day in males.[21] In other studies, 25 mg/day CPA resulted in substantial improvement or complete clearance of severe acne in almost all males, whereas 12.5 mg/day was ineffective.[61][62]
CPA has been found to be strongly catabolic in young healthy males.[57][63] It was shown to result in a mean negative nitrogen balance of 1.2 g at 50 mg/day, 1.4 g at 100 mg/day, and 2.5 g at 200 mg/day.[57][63] This corresponded to mean losses of lean tissue of 780, 945, and 1,515 g, respectively.[63] Conversely, the catabolic effect was much less in an older male, and no such effect was observed in adult females consuming a diet with sufficient calories and protein.[57][63] The catabolic effects of CPA were found to be greater than those of corticosteroids.[63]
Although higher doses of CPA are necessary for considerable systemic AR antagonistic activity, it is notable that even low doses of oral CPA appear to be able to significantly antagonize AR signaling in the liver in women.[64] This may be related to the hepatic first-pass effect of oral administration, and is evidenced by the fact that whereas combined birth control pills containing CPA increase SHBG levels by 300 to 400%, combined birth control pills containing various other progestins, with either androgenic or antiandrogenic activity, increase SHBG levels by only 50 to 300%.[64] This is relevant as estrogens stimulate hepatic SHBG production while androgens inhibit hepatic SHBG production, and vice versa for their antagonists.[1][65] The antiandrogenic activity of CPA may also be responsible for the relatively greater risk of venous thromboembolism with CPA-containing birth control pills compared to those containing other progestins.[66]
In rats, a dosage of CPA of 25 mg/kg/day results in complete regression of prostate gland growth in gonadally intact males.[49] The equivalent dosage in humans, on the basis of body surface (conversion factor from rat to human of 6), was estimated to be approximately 4 mg/kg/day, or around 300 mg/day CPA for a 75 kg (165 lb) man.[49] Other techniques for determining the dosage of CPA have validated this extrapolation, for instance affinity studies and prostatic CPA levels.[49] The affinity of CPA for the AR is around 20-fold lower than that of DHT, and an excess of CPA levels of around 20 to 30 times those of DHT would hence be expected to maximally neutralize androgen signaling.[49] In accordance, different publications have stated based on preclinical experiments that a 2- to 5-fold excess of CPA can inhibit the effects of testosterone by 50%, a 3- to 10-fold excess of CPA can reduce the effects of "potent androgens" (presumably testosterone and/or DHT) by 50%, and a 10-fold excess of CPA can inhibit the effects of testosterone by "almost 100%".[67][68][69] High-dose CPA has been found to achieve prostatic levels that are at least 30-fold those of DHT.[49] One study found that levels of CPA in the prostate gland in men being treated with 200 mg/day oral CPA were about 28 times those of DHT.[49] In accordance with the preceding findings, it has been stated that oral doses of CPA of at least 300 mg/day may achieve a combined androgen blockade action in the treatment of prostate cancer.[70] At a dosage of CPA of 100 mg/day in men with prostate cancer, circulating levels of CPA (e.g., 350 ng/mL) are on the order of 200-fold higher than circulating levels of testosterone (e.g., 100 ng/dL).[71] In men who have undergone orchiectomy, 50 mg/day oral CPA results in a 500-fold excess of circulating CPA relative to circulating testosterone.[71]
In accordance with such findings, high-dose CPA shows equivalent effects on the prostate gland in men relative to high-dose diethylstilbestrol or buserelin, which both achieve castrate levels of testosterone.[49] However, a lower dosage of 50 mg/day CPA has been found to produce a reduction in prostate volume in men with benign prostatic hyperplasia that is reportedly comparable to that observed with surgical or medical castration.[49] In accordance, the dosage of CPA that achieves complete inhibition of the secretory function of the healthy prostate gland is around 50 to 100 mg/day, which is less than the dosage of 200 to 300 mg/day CPA that is used to treat prostate cancer.[72] It has been said that in combined androgen blockade regimens with castration and CPA as the AR antagonist for prostate cancer, due to the marked reduction in androgen levels, lower dosages of CPA than those used as a monotherapy would seem to be equally effective.[49] Relative to the 200 to 300 mg/day dosage of CPA used as a monotherapy in prostate cancer, the recommended dosage in combined androgen blockade is 100 to 200 mg/day.[72] It has been stated that this dosage should be more than necessary to inhibit the effects of the remaining adrenal androgens in castrated men.[72]
Despite considerable suppression of testosterone levels, only a modest suppression of spermatogenesis typically occurs with 5 to 10 mg/day CPA, and azoospermia occurs only occasionally.[73] Conversely, a combination of testosterone enanthate injections with 12.5 to 100 mg/day CPA results in azoospermia in most men.[73][74] The rates of azoospermia increased with greater CPA dosage, which was attributed to the additional AR antagonism of higher doses of CPA.[73][74] Significant spermatogenesis still occurs with 50 mg/day CPA alone, but spermatogenesis is significantly reduced compared to normal.[75] At a dosage of 200 mg/day, CPA has been found to produce azoospermia (sperm count of less than 1 million/mL) in men within 8 to 10 weeks of treatment.[75] However, fertility is generally lost even at a lower dosage of CPA of 100 mg/day because there is complete inhibition of the accessory sex glands and hence an absence of semen production and ejaculate upon orgasm.[75][72][57] Ejaculate volume decreases at a dosage of 50 mg/day and decreases to almost zero after 6 weeks of high-dose CPA therapy.[57][68] The effects of CPA on fertility are completely reversible.[72] This has been demonstrated in clinical studies of male adolescents and adults treated with CPA continuously for 6 to 7 years.[72]
Weak partial androgenic activity
CPA, like spironolactone and other steroidal antiandrogens such as chlormadinone acetate and megestrol acetate, is actually not a pure antagonist of the AR – that is, a silent antagonist – but rather appears to be a very weak partial agonist.[56][15][76][77][78][79][80] Clinically, CPA generally functions purely as an antiandrogen, as it displaces much more efficacious endogenous androgens such as testosterone and DHT from interacting with the receptor and thus its net effect is virtually always to lower physiological androgenic activity.[49][81] But unlike silent antagonists of the AR like nonsteroidal antiandrogens such as flutamide, bicalutamide, and enzalutamide, CPA, by virtue of its slight intrinsic activity at the AR, may be unable to fully inhibit androgenic signaling in the body, which may persist to an extent in some tissues such as the prostate gland.[56]
In accordance with its albeit weak capacity for activation of the AR, CPA has been found to stimulate androgen-sensitive carcinoma growth in the absence of other androgens, an effect which could be blocked by co-treatment with flutamide.[56][78][79] In one study in rodents, DHT-stimulated prostate weight remained 40% above controls with administration of CPA even at the highest dosage, while flutamide was able to completely block the stimulatory effects of DHT.[82] In addition, CPA alone increased prostate weight by 60%, whereas flutamide had no effect.[82] As a result of its weak intrinsic androgenicity, CPA may not be as effective in the treatment of certain androgen-sensitive conditions such as prostate cancer compared to nonsteroidal antiandrogens with a silent antagonist profile at the AR.[15][83] Indeed, CPA has never been found to extend life in prostate cancer patients when added to castration relative to castration alone, unlike nonsteroidal antiandrogens.[84] As such, it is thought that the partial androgenic activity of CPA and other steroidal antiandrogens underlies the superior antiandrogenic efficacy of silent-antagonist nonsteroidal antiandrogens like flutamide.[76] However, the clinical significance of the weak androgenic activity of CPA has also been disputed.[49][85][86] In fact, some studies have found little or no stimulating effect of CPA on the prostate gland or seminal vesicles of male rats even with very high circulating concentrations of CPA.[85][86]
Nonsteroidal antiandrogens like flutamide and bicalutamide are more efficacious as antiandrogens than CPA in castrated animals due to their superior AR antagonistic activity.[72][87] Conversely, CPA is a much more potent antiandrogen than nonsteroidal antiandrogens like flutamide and bicalutamide in gonadally intact male animals, which is due to its antigonadotropic effects and consequent suppression of testosterone levels (nonsteroidal antiandrogens do not suppress testosterone levels).[72][87]
CPA at high doses in combination with transdermal estradiol gel has been reported to suppress SHBG levels in women and may have a partial androgenic effect on hepatic SHBG production at such doses.[88][89] Likewise, high-dose CPA alone in men has been reported to significantly decrease SHBG levels.[90] Similar effects are known for related progestins like medroxyprogesterone acetate and megestrol acetate.[1] CPA has also been reported to lower HDL cholesterol levels, another effect associated with androgens.[91] Accordingly, CPA shows weak androgenic effects in the liver in rodents which can be blocked by flutamide.[92][93]
Other androgenic and antiandrogenic actions
A paradoxical effect occurs with certain prostate cancer cells which have genetic mutations in their ARs.[94][95][96] These altered ARs can be activated, rather than inhibited, by CPA.[94][95][96] In such cases, withdrawal of CPA may result in a reduction in cancer growth, rather than the reverse.[94][95][96] This is known as antiandrogen withdrawal syndrome.[94][95][96]
CPA may also have a slight direct inhibitory effect on 5α-reductase, though the evidence for this is sparse and conflicting.[97][98][99] Most studies however suggest that CPA does not produce important inhibition of 5α-reductase.[68][100][59] The combination of birth control pills containing CPA with finasteride, a well-established, selective 5α-reductase inhibitor, has been found to result in significantly improved effectiveness in the treatment of hirsutism relative to CPA-containing birth control pills alone.[101][102]
In addition to its AR antagonistic activity and suppression of gonadal sex-hormone production, high-dose CPA has been found to suppress the levels of the adrenal androgen dehydroepiandrosterone sulfate (DHEA-S), which is due to exertion of negative feedback by CPA on adrenocorticotropic hormone (ACTH) secretion via the glucocorticoid activity of CPA.[56][67][23]
Progestogenic activity
CPA is a highly potent progestogen.[103] It is described as the most potent progestin of the 17α-hydroxyprogesterone group, being about 1,200-fold more potent than hydroxyprogesterone acetate, 12-fold more potent than medroxyprogesterone acetate, and 3-fold more potent than chlormadinone acetate in animal bioassays.[57][41] Based on results in the animal bioassays, CPA has also been said to be the most potent progestin known, with 1,000 times the potency of progesterone.[57] With oral administration in humans however, CPA is distinctly less potent as a progestogen than various other progestins such as the 19-nortestosterone derivatives.[1] The effective dosage of CPA needed to inhibit ovulation by itself in women (i.e., to act as a contraceptive) is 1 mg/day,[1] and the medication is marketed as a contraceptive (combined with low-dose ethinylestradiol) at a dosage of 2 mg/day.[21][103][55] For comparison, the ovulation-inhibiting dosage of levonorgestrel is 50 μg/day.[1]
At the dosages typically used clinically, CPA is described as a "strong" and "powerful" progestogen.[104][21][105] Its endometrial transformation dosage is 20 to 30 mg per cycle and its menstrual delay test dosage has been estimated to be less than 1 mg/day.[21] CPA is not well-balanced in terms of its activities; relative to the progestogenic potency of CPA, its potency as an androgen receptor antagonist is quite weak.[21] In order to take full advantage of its antiandrogenic activity, CPA must be administered at a dosage of 50 to 100 mg per day, which is 2 to 3 times the cyclical endometrial transformation dose per day.[21][106][105] As such, the total dosage of CPA per month is as much as 30 times the physiological equivalent of progesterone production during the normal menstrual cycle, and is notably equivalent to the total production of progesterone by a corpus luteum throughout the course of a woman's entire cyclic life.[21][106][105] Consequently, there is profound overdosage of progestogenic effect (and by extension progestogenic side effects) when CPA is used as an antiandrogen at high doses.[106][105] For this reason, it has been said that CPA cannot be considered an ideal antiandrogen.[106][105]
Through its action as a progestogen, CPA has been found to significantly increase prolactin secretion and to induce extensive lobuloalveolar development of the mammary glands of female rhesus macaques.[107] In accordance, a study found that CPA, in all cases, induced full lobuloalveolar development of the breasts in transgender women treated with the medication in combination with estrogen for a prolonged period of time.[108][109][110] Pregnancy-like breast hyperplasia was observed in two of the subjects.[110] In contrast, the same study found that men with prostate cancer treated with a non-progestogenic antiandrogen like flutamide or bicalutamide and no estrogen produced moderate but incomplete lobuloalveolar development of the breasts.[108] Based on the above research, it was concluded by the study authors that combined estrogenic and progestogenic action is required in transgender women for fully mature female-like histologic breast development (i.e., that includes complete lobuloalveolar maturation).[108][109] Also, it was observed that lobuloalveolar maturation reverses upon discontinuation of CPA after surgical castration, similarly to the case of mammary gland involution in postpartum women, indicating that continued progestogen treatment is necessary to maintain the histology.[108] It should be noted however that although these findings may have important implications in the context of lactation and breastfeeding, epithelial tissue accounts for approximately only 10% of breast volume with the bulk of the breasts (80–90%) being represented by stromal or adipose tissue,[111][112][113][114] and it is uncertain to what extent, if any, that development of lobuloalveolar structures (a type of epithelial tissue) contributes to breast size or shape.[115]
CPA has been found to increase prolactin levels in humans both alone and in combination with an estrogen.[116]
Antigonadotropic effects
CPA has potent antigonadotropic effects via its progestogenic activity.[13][117][103][15] It blunts the gonadotropin releasing hormone (GnRH)-induced secretion of gonadotropins, and accordingly, markedly suppresses circulating levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) at sufficiently high doses.[13][118] Consequently, levels of progesterone, androstenedione, testosterone, DHT, and estradiol are also markedly lowered at sufficiently high dosages, while an elevation in sex hormone-binding globulin (SHBG) and prolactin levels is observed.[119][120][121][122][123]
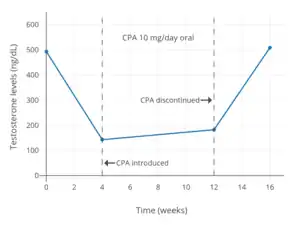
The effective dosage of CPA for inhibition of ovulation in women, this being an antigonadotropic effect, is 1 mg/day.[1] Oral CPA has been studied at low dosages of 5 to 20 mg/day as a potential male hormonal contraceptive.[124][125] A dosage of as low as 5 to 10 mg/day oral CPA has been found to suppress circulating testosterone levels in men by 50 to 70%.[126][119][127][128] For comparison with lower dosages, the suppression of circulating testosterone levels in men with a dosage of 100 mg/day oral CPA was 77% and with a dosage of 300 mg/week intramuscular CPA was 76%.[129][130] Dosages of CPA of 12.5 to 25 mg/day have been used as a maintenance dosage for testosterone suppression in men with sexual deviance after initial administration of higher CPA dosages, without recurrence of symptoms.[131][132] CPA is generally able to maximally suppress circulating testosterone levels by 70 to 80% in men.[57][133][87] However, in spite of strong suppression of testosterone levels, CPA, at least by itself (e.g., without estrogen), is not usually able to reduce testosterone levels into the castrate/female range (<50 ng/dL) at any dosage, and testosterone levels generally remain just above it at levels of roughly 50 to 200 ng/dL.[57][134][87][129][135] However, studies have reported that a very high dosage of CPA of 300 mg/day may suppress testosterone levels to around 50 ng/dL in men.[69][136] CPA also suppresses estradiol levels in men, with one study finding about a 65% decrease in estradiol levels (from about 27 pg/mL to around 10 pg/mL) with 100 mg/day CPA.[69]
CPA has been found to maximally suppress testosterone and estradiol levels in young men within 7 days of continuous administration.[11] Following discontinuation of CPA, the recovery of testosterone levels is variable and may require 14 days to 6 months for completion.[67] An escape or recovery phenomenon, in which testosterone levels increase over time, has been observed with long-term CPA monotherapy.[137][71] In one study in aged men with prostate cancer, testosterone levels were initially suppressed by 70%, but increased to 50% of baseline levels between 6 and 12 months, remaining stable thereafter up to 24 months of therapy.[137][71]
The combination of progestogens like CPA with an estrogen is synergistic in terms of antigonadotropic effect, and is able to fully suppress gonadal testosterone production even with very small doses of the estrogen.[87][138][139][140][141] One study found that 100 to 300 mg/day CPA combined with an "extremely low" dosage of diethylstilbestrol (0.1 mg/day), a nonsteroidal estrogen, suppressed testosterone levels into the castrate range (to 30 ng/dL) in men with prostate cancer.[87][142][143] Discontinuation of diethylstilbestrol at 5 months resulted in a rapid 6-fold increase in testosterone levels (to 135 ng/dL) and then further (to almost 200 ng/dL) by 12 months.[142] Another study likewise found that the combination of 160 mg/day oral megestrol acetate, a progestin closely related to CPA, with 0.5 to 1.5 mg/day oral estradiol suppressed testosterone levels into the castrate range in men with prostate cancer.[138] A study by Fung and colleagues (2017) found no difference in suppression of circulating testosterone levels (~95% suppression) in transgender women by the combination of either 25 mg/day oral CPA or 50 mg/day oral CPA with a moderate dosage of oral or transdermal estradiol (mean 3.3 mg/day oral, 3.4 g/day gel, or 95.6 μg/day patches).[140]
A high dosage of CPA given starting 7 days prior to initiation of GnRH agonist therapy was found to prevent the GnRH agonist-induced flare in testosterone levels.[11] The combination of 100 mg/day CPA and 0.1 mg/day diethylstilbestrol given starting 4 weeks before GnRH-agonist introduction has also been found to prevent the GnRH agonist-induced testosterone flare.[144] CPA should be given continuously for at least a week prior to GnRH agonist initiation for an optimal preventative effect on the GnRH agonist-induced testosterone flare.[11]
- Testosterone levels with cyproterone acetate

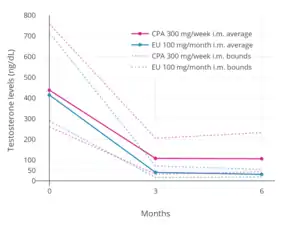 Testosterone levels with 300 mg/week cyproterone acetate or 100 mg/month estradiol undecylate both by intramuscular injection in men.[129] Solid lines are average and dashed lines highest and lowest levels. Levels of testosterone decreased by 75% with cyproterone acetate and by 91% with estradiol undecylate.[129]
Testosterone levels with 300 mg/week cyproterone acetate or 100 mg/month estradiol undecylate both by intramuscular injection in men.[129] Solid lines are average and dashed lines highest and lowest levels. Levels of testosterone decreased by 75% with cyproterone acetate and by 91% with estradiol undecylate.[129]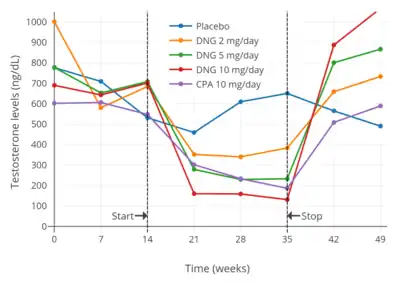


 Testosterone levels with 100 to 300 mg/day oral cyproterone acetate and low-dose oral estrogen in men.[142] The estrogen used was 0.1 mg/day diethylstilbestrol (DES),[142] which has been described as an "extremely low" dosage.[87] Levels of testosterone were decreased by about 95% with the combination and by about 61% with cyproterone acetate only.[142]
Testosterone levels with 100 to 300 mg/day oral cyproterone acetate and low-dose oral estrogen in men.[142] The estrogen used was 0.1 mg/day diethylstilbestrol (DES),[142] which has been described as an "extremely low" dosage.[87] Levels of testosterone were decreased by about 95% with the combination and by about 61% with cyproterone acetate only.[142]
 Testosterone levels with estradiol (E2) alone or in combination with an antiandrogen (AA) in the form of spironolactone (SPL) or cyproterone acetate (CPA) in transfeminine people.[150] Estradiol was used in the form of oral estradiol valerate (EV) in almost all cases.[150] The dashed horizontal line is the upper limit of the female/castrate range (~50 ng/dL).
Testosterone levels with estradiol (E2) alone or in combination with an antiandrogen (AA) in the form of spironolactone (SPL) or cyproterone acetate (CPA) in transfeminine people.[150] Estradiol was used in the form of oral estradiol valerate (EV) in almost all cases.[150] The dashed horizontal line is the upper limit of the female/castrate range (~50 ng/dL).
Glucocorticoid activity
CPA is an agonist of the glucocorticoid receptor (GR), and has weak and partial glucocorticoid activity at high doses.[1][67][72] In animals, CPA suppresses the secretion of adrenocorticotropic hormone (ACTH) from the pituitary gland, suppresses the production of corticosteroids like cortisol and corticosterone by the adrenal cortices, and decreases the weights of the adrenal glands and thymus.[68][72] Conversely however, CPA shows no anti-inflammatory or eosinophilic effects in animals.[68][72] As such, CPA, as well as related antiandrogens, show only some of the typical effects of glucocorticoids.[68][72] CPA may produce mild glucucorticoid actions at high doses of more than 100 mg/day in humans.[151] Clinically, the glucocorticoid effects of CPA appear to be relevant only at high doses in people with small body sizes (CPA exposure of more than 80 to 100 mg/m2), namely in the treatment of children with precocious puberty.[68][72] No signs of secondary adrenal insufficiency have been observed with CPA.[68][72] While various studies have clearly shown reduced cortisol and ACTH levels and ACTH responsiveness in humans with CPA therapy, some studies contradict these findings and report no such effects even with high doses of CPA.[152][153][154][155][156][85]
Due to negative feedback on the hypothalamic–pituitary-adrenal (HPA) axis, administration of exogenous glucocorticoids such as prednisone and dexamethasone suppress the secretion of adrenocorticotropic hormone (ACTH) from the pituitary gland and the production of cortisol from the adrenal glands. This results in adrenal suppression and atrophy and, upon glucocorticoid discontinuation, temporary adrenal insufficiency. Similarly, CPA both in animals and humans can weakly reduce ACTH and cortisol levels and decrease adrenal gland weight as well as cause adrenal insufficiency with discontinuation. These findings suggest that CPA possesses weak glucocorticoid properties.[157][158][159][160][161][162][163] CPA has been reported to be an antagonist of the glucocorticoid receptor (GR) in vitro[16][164][165] and may reduce adrenal cortisol and corticosterone production by weakly inhibiting the enzymes 3β-hydroxysteroid dehydrogenase and 21-hydroxylase.[159][166][167][168] These are antiglucocorticoid actions. However, metabolites of CPA, for instance 15β-hydroxycyproterone acetate, may have differing activities.[9][169][152] Both cyproterone and CPA have been found to possess glucocorticoid effects, and based on studies in mice, it has been suggested that CPA has approximately one-fifth of the potency of prednisone as a glucocorticoid.[170] The glucocorticoid effects of CPA in humans appear to be less significant than those in animals.[152]
Megestrol acetate, medroxyprogesterone acetate, and chlormadinone acetate are all steroidal progestins of the 17α-hydroxyprogesterone family and close analogues of CPA which similarly possess glucocorticoid properties and the potential for producing adrenal insufficiency upon discontinuation.[171][172]
Estrogenic and antiestrogenic activities
CPA does not bind to the estrogen receptors.[1] Accordingly, pre-treatment with CPA does not block the retention of estradiol in the brain in mice.[173] CPA has no estrogenic or direct antiestrogenic activity.[1] However, CPA has been reported to produce weak estrogenic effects in rodents.[174][175][176] In any case, CPA has prominent indirect antiestrogenic effects via its progestogenic activity.[1] This includes PR-mediated antiestrogenic activity in certain tissues like the uterus and vagina as well as suppression of estrogen levels via its PR-mediated antigonadotropic activity.[1] CPA also has indirect estrogenic activity in the breasts via its antiandrogenic activity, as androgens have strong functional antiestrogenic effects in this part of the body. This underlies the slight gynecomastia that can occur with CPA in men.
Opioid receptors
CPA has been found to bind to several of the opioid receptors, including the μ-, δ-, and κ-opioid receptor subtypes.[177][178] However, this binding is very weak relative to its other actions (IC50 for inhibition of [3H]diprenorphine binding = 1.62 ± 0.33 μM).[177][178] It has been suggested that activation of opioid receptors might be involved in the sedation that is reportedly sometimes seen with high doses of CPA or in its reported effectiveness in the treatment of cluster headaches.[177]
Pharmacokinetics
Absorption
The oral bioavailability of CPA is 68 to 100%.[1][2] The absorption of oral CPA is slow but complete, and the medication is not subject to a significant first-pass effect.[67][179] The mean absorption half-life of oral CPA is about 1.5 hours.[67] Steady-state levels of CPA occur with oral CPA after about 8 days of continuous administration, with a 2- to 3-fold gradual accumulation in CPA levels.[67] Oral CPA is taken daily and intramuscular CPA is administered weekly or biweekly.[180]
Following a single low oral dose of 2 mg CPA in combination with 35 or 50 μg ethinylestradiol in premenopausal women, mean peak levels of CPA of 7.2 to 15.2 ng/mL (17–36.5 nmol/L) have been recorded after 1.6 to 3.7 hours.[47][181][182][183][184] In healthy men, a single high oral dose of 100 mg CPA produced maximal CPA levels of 254 ng/mL (609 nmol/L) after 2.6 hours.[185] In aged men with prostate cancer, continuous oral CPA therapy resulted in CPA levels of 132 ± 18 ng/mL at 25 mg/day, 246 ± 13 ng/mL at 50 mg/day, and 348 ± 23 ng/mL at 100 mg/day.[71] Similarly, in healthy young women, a single high oral dose of 100 mg CPA resulted in peak CPA levels of 255 ng/mL (612 nmol/L) within 2 to 3 hours.[2][186] During continuous treatment with high oral doses of CPA in women with hirsutism, levels of CPA were 199 to 228 ng/mL (477–547 nmol/L) with 50 mg/day CPA and were 436 to 520 ng/mL (1050–1250 nmol/L) with 100 mg/day CPA.[187]
After a single intramuscular injection of 300 mg CPA in healthy young women, maximal levels of CPA of 191 ng/mL (458 nmol/L) and of 15β-OH-CPA of 164 ng/mL occurred after 2 to 4 days.[2][186] During continuous weekly intramuscular injections of CPA in men with prostate cancer, mean levels of CPA roughly doubled from 170 ng/mL (408 nmol/L) after the first injection to 310 ng/mL (744 nmol/L) after the fifth injection, and were projected to increase to 350 to 400 ng/mL (840–960 nmol/L) after around 8 to 12 injections.[120] The area-under-the-curve (AUC; total exposure) levels of CPA with 100 mg/day oral CPA and 300 mg/week intramuscular CPA may be approximately equivalent.[120]
- Cyproterone acetate levels with oral and intramuscular cyproterone acetate
Distribution
With oral CPA, there is a probable distribution phase of CPA into tissues which lasts about 12 hours and has a half-life of 3 hours.[67] CPA is very lipophilic, and it is sequestered into fat, which provides a depot effect.[11][67][47] The volume of distribution of CPA is 20.6 ± 3.5 L/kg.[2][186] CPA crosses the blood–brain barrier, which is evidenced by the suppression of gonadotropin secretion that is observed during therapy with it (the site of action of this effect being the pituitary gland, a part of the brain).[191] In terms of plasma protein binding, CPA does not bind to SHBG or corticosteroid-binding globulin[192] and is instead bound exclusively to albumin (93%), with the remainder (7%) circulating free or unbound.[1][3][4][5][6] The affinity of CPA for SHBG is very low at about 0.006% of that of testosterone or DHT.[67]
Metabolism
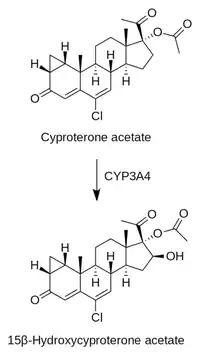
CPA is metabolized primarily by hydroxylation via CYP3A4, forming the major active metabolite 15β-hydroxycyproterone acetate.[1][9] This metabolite circulates at concentrations approximately twice those of CPA, and has similar antiandrogen activity to that of CPA but only 10% of its activity as a progestogen.[1][9][195][196] As a result, the co-administration of CPA with drugs which inhibit CYP3A4 may increase its potency as a progestogen.[3]
Some CPA is reportedly metabolized by hydrolysis into cyproterone and acetic acid.[197] However, unlike many other steroid esters, CPA is not extensively hydrolyzed, and much of the pharmacological activity of the drug is attributable to CPA itself in its unchanged form.[198] Cyproterone has approximately one-third the potency of CPA as an antiandrogen[199] and is devoid of progestogenic activity.[57]
The elimination half-life of oral CPA is relatively long at approximately 1.6 to 2.2 days (38 to 53 hours), but possibly as long as 3.6 to 4.3 days (86 to 100 hours).[1][11][200][2][186] The half-life of 15β-OH-CPA with oral administration of CPA is 2.6 days.[2][186] The elimination half-life of CPA is prolonged in obese patients, which may be due to relatively greater storage of CPA in fat.[67] The elimination half-life of CPA is also longer in older individuals; it is approximately twice as long in elderly men than in younger men (95 hours and 45 hours, respectively).[185] When given via depot intramuscular injection, CPA has an elimination half-life of 3 to 4.3 days while 15β-OH-CPA has a half-life of 5.2 days.[2][10][12][186] The duration of action of a single intramuscular injection of CPA is about 14 to 20 days.[39][37][38] The serum total clearance of CPA is approximately 2.32 ± 0.38 mL/min/kg.[2][186] Levels of CPA and 15β-OH-CPA with oral administration decrease biphasically over a period of 24 to 120 hours.[2][186]
References
- Kuhl H (2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration" (PDF). Climacteric. 8 Suppl 1: 3–63. doi:10.1080/13697130500148875. PMID 16112947. S2CID 24616324.
- Huber J, Zeillinger R, Schmidt J, Täuber U, Kuhnz W, Spona J (November 1988). "Pharmacokinetics of cyproterone acetate and its main metabolite 15 beta-hydroxy-cyproterone acetate in young healthy women". Int J Clin Pharmacol Ther Toxicol. 26 (11): 555–61. PMID 2977383.
- Bińkowska M, Woroń J (June 2015). "Progestogens in menopausal hormone therapy". Przegla̜d Menopauzalny = Menopause Review. 14 (2): 134–43. doi:10.5114/pm.2015.52154. PMC 4498031. PMID 26327902.
- Schindler AE, Campagnoli C, Druckmann R, Huber J, Pasqualini JR, Schweppe KW, Thijssen JH (December 2003). "Classification and pharmacology of progestins" (PDF). Maturitas. 46 Suppl 1: S7–S16. doi:10.1016/j.maturitas.2003.09.014. PMID 14670641.
Since there is no binding of CPA to SHBG and CBG in the serum, 93% of the compound is bound to serum albumin.
- Wakelin SH, Maibach HI, Archer CB (1 June 2002). Systemic Drug Treatment in Dermatology: A Handbook. CRC Press. pp. 32–. ISBN 978-1-84076-013-2.
It is almost exclusively bound to plasma albumin.
- Hammond GL, Lähteenmäki PL, Lähteenmäki P, Luukkainen T (October 1982). "Distribution and percentages of non-protein bound contraceptive steroids in human serum". Journal of Steroid Biochemistry. 17 (4): 375–80. doi:10.1016/0022-4731(82)90629-X. PMID 6215538.
- Dickman A (27 September 2012). Drugs in Palliative Care. OUP Oxford. pp. 137–138. ISBN 978-0-19-966039-1.
- Boarder M, Newby D, Navti P (25 March 2010). Pharmacology for Pharmacy and the Health Sciences: A Patient-centred Approach. OUP Oxford. pp. 632–. ISBN 978-0-19-955982-4.
- Frith RG, Phillipou G (1985). "15-Hydroxycyproterone acetate and cyproterone acetate levels in plasma and urine". J. Chromatogr. 338 (1): 179–86. doi:10.1016/0378-4347(85)80082-7. PMID 3160716.
- Weber GF (22 July 2015). Molecular Therapies of Cancer. Springer. pp. 316–. ISBN 978-3-319-13278-5.
The terminal half-life is about 38 h. A portion of the drug is metabolized by hydrolysis to cyproterone and acetic acid. However, in contrast to many other steroid esters hydrolysis is not extensive, and much of the pharmacological activity is exerted by the acetate form. Excretion is about 70% in the feces, mainly in the form of glucuronidated metabolites, and about 30% in the urine, predominantly as non-conjugated metabolites.
- Barradell LB, Faulds D (July 1994). "Cyproterone. A review of its pharmacology and therapeutic efficacy in prostate cancer". Drugs Aging. 5 (1): 59–80. doi:10.2165/00002512-199405010-00006. PMID 7919640.
- AAPL Newsletter (PDF). The Academy. 1998.
CPA is 100% bioavailable when taken orally with a half life of 38 hours. The injectable form reaches maximum plasma levels in 82 hours and has a half life of about 72 hours.
- Neumann F (1994). "The antiandrogen cyproterone acetate: discovery, chemistry, basic pharmacology, clinical use and tool in basic research". Exp. Clin. Endocrinol. 102 (1): 1–32. doi:10.1055/s-0029-1211261. PMID 8005205.
- Berek JS (2007). Berek & Novak's Gynecology. Lippincott Williams & Wilkins. p. 1085. ISBN 978-0-7817-6805-4.
- Figg W, Chau CH, Small EJ (14 September 2010). Drug Management of Prostate Cancer. Springer. p. 71. ISBN 978-1-60327-829-4.
- Honer C, Nam K, Fink C, Marshall P, Ksander G, Chatelain RE, Cornell W, Steele R, Schweitzer R, Schumacher C (May 2003). "Glucocorticoid receptor antagonism by cyproterone acetate and RU486". Molecular Pharmacology. 63 (5): 1012–20. doi:10.1124/mol.63.5.1012. PMID 12695529. S2CID 23872584.
- Ayub M, Levell MJ (July 1987). "Inhibition of rat testicular 17 alpha-hydroxylase and 17,20-lyase activities by anti-androgens (flutamide, hydroxyflutamide, RU23908, cyproterone acetate) in vitro". Journal of Steroid Biochemistry. 28 (1): 43–7. doi:10.1016/0022-4731(87)90122-1. PMID 2956461.
- Han C, Davis CB, Wang B (6 January 2010). Evaluation of Drug Candidates for Preclinical Development: Pharmacokinetics, Metabolism, Pharmaceutics, and Toxicology. John Wiley & Sons. pp. 92–. ISBN 978-0-470-57488-1.
- Lehmann JM, McKee DD, Watson MA, Willson TM, Moore JT, Kliewer SA (September 1998). "The human orphan nuclear receptor PXR is activated by compounds that regulate CYP3A4 gene expression and cause drug interactions". The Journal of Clinical Investigation. 102 (5): 1016–23. doi:10.1172/JCI3703. PMC 508967. PMID 9727070.
- Christians U, Schmitz V, Haschke M (December 2005). "Functional interactions between P-glycoprotein and CYP3A in drug metabolism". Expert Opinion on Drug Metabolism & Toxicology. 1 (4): 641–54. doi:10.1517/17425255.1.4.641. PMID 16863430. S2CID 17742146.
- Hammerstein, J. (1990). "Antiandrogens: Clinical Aspects". Hair and Hair Diseases. pp. 827–886. doi:10.1007/978-3-642-74612-3_35. ISBN 978-3-642-74614-7.
- Rittmaster RS (June 1999). "Antiandrogen treatment of polycystic ovary syndrome". Endocrinol. Metab. Clin. North Am. 28 (2): 409–21. doi:10.1016/S0889-8529(05)70077-3. PMID 10352926.
- Diamanti-Kandarakis E (September 1999). "Current aspects of antiandrogen therapy in women". Curr. Pharm. Des. 5 (9): 707–23. PMID 10495361.
- Knörr K, Beller FK, Lauritzen C (17 April 2013). Lehrbuch der Gynäkologie. Springer-Verlag. pp. 214–. ISBN 978-3-662-00942-0.
- Knörr K, Knörr-Gärtner H, Beller FK, Lauritzen C (8 March 2013). Geburtshilfe und Gynäkologie: Physiologie und Pathologie der Reproduktion. Springer-Verlag. pp. 583–. ISBN 978-3-642-95583-9.
- A. Labhart (6 December 2012). Clinical Endocrinology: Theory and Practice. Springer Science & Business Media. pp. 554–. ISBN 978-3-642-96158-8.
- Horský J, Presl J (1981). "Hormonal Treatment of Disorders of the Menstrual Cycle". In Horsky J, Presl K (eds.). Ovarian Function and its Disorders: Diagnosis and Therapy. Springer Science & Business Media. pp. 309–332. doi:10.1007/978-94-009-8195-9_11. ISBN 978-94-009-8195-9.
- Joachim Ufer (1969). The Principles and Practice of Hormone Therapy in Gynaecology and Obstetrics. de Gruyter. p. 49.
17α-Hydroxyprogesterone caproate is a depot progestogen which is entirely free of side actions. The dose required to induce secretory changes in primed endometrium is about 250 mg. per menstrual cycle.
- Willibald Pschyrembel (1968). Praktische Gynäkologie: für Studierende und Ärzte. Walter de Gruyter. pp. 598, 601. ISBN 978-3-11-150424-7.
- Ferin J (September 1972). "Effects, Duration of Action and Metabolism in Man". In Tausk M (ed.). Pharmacology of the Endocrine System and Related Drugs: Progesterone, Progestational Drugs and Antifertility Agents. II. Pergamon Press. pp. 13–24. ISBN 978-0080168128. OCLC 278011135.
- Henzl MR, Edwards JA (10 November 1999). "Pharmacology of Progestins: 17α-Hydroxyprogesterone Derivatives and Progestins of the First and Second Generation". In Sitruk-Ware R, Mishell DR (eds.). Progestins and Antiprogestins in Clinical Practice. Taylor & Francis. pp. 101–132. ISBN 978-0-8247-8291-7.
- Janet Brotherton (1976). Sex Hormone Pharmacology. Academic Press. p. 114. ISBN 978-0-12-137250-7.
- Sang GW (April 1994). "Pharmacodynamic effects of once-a-month combined injectable contraceptives". Contraception. 49 (4): 361–85. doi:10.1016/0010-7824(94)90033-7. PMID 8013220.
- Toppozada MK (April 1994). "Existing once-a-month combined injectable contraceptives". Contraception. 49 (4): 293–301. doi:10.1016/0010-7824(94)90029-9. PMID 8013216.
- Bagade O, Pawar V, Patel R, Patel B, Awasarkar V, Diwate S (2014). "Increasing use of long-acting reversible contraception: safe, reliable, and cost-effective birth control" (PDF). World J Pharm Pharm Sci. 3 (10): 364–392. ISSN 2278-4357. Archived from the original (PDF) on 10 August 2017. Retrieved 24 August 2016.
- Goebelsmann U (1986). "Pharmacokinetics of Contraceptive Steroids in Humans". In Gregoire AT, Blye RP (eds.). Contraceptive Steroids: Pharmacology and Safety. Springer Science & Business Media. pp. 67–111. doi:10.1007/978-1-4613-2241-2_4. ISBN 978-1-4613-2241-2.
- Becker H, Düsterberg B, Klosterhalfen H (1980). "[Bioavailability of cyproterone acetate after oral and intramuscular application in men (author's transl)]" [Bioavailability of Cyproterone Acetate after Oral and Intramuscular Application in Men]. Urologia Internationalis. 35 (6): 381–5. doi:10.1159/000280353. PMID 6452729.
- Moltz L, Haase F, Schwartz U, Hammerstein J (May 1983). "[Treatment of virilized women with intramuscular administration of cyproterone acetate]" [Efficacy of Intra muscularly Applied Cyproterone Acetate in Hyperandrogenism]. Geburtshilfe Und Frauenheilkunde. 43 (5): 281–7. doi:10.1055/s-2008-1036893. PMID 6223851.
- Wright JC, Burgess DJ (29 January 2012). Long Acting Injections and Implants. Springer Science & Business Media. pp. 114–. ISBN 978-1-4614-0554-2.
- Chu YH, Li Q, Zhao ZF (April 1986). "Pharmacokinetics of megestrol acetate in women receiving IM injection of estradiol-megestrol long-acting injectable contraceptive". The Chinese Journal of Clinical Pharmacology.
The results showed that after injection the concentration of plasma MA increased rapidly. The meantime of peak plasma MA level was 3rd day, there was a linear relationship between log of plasma MA concentration and time (day) after administration in all subjects, elimination phase half-life t1/2β = 14.35 ± 9.1 days.
- Runnebaum BC, Rabe T, Kiesel L (6 December 2012). Female Contraception: Update and Trends. Springer Science & Business Media. pp. 429–. ISBN 978-3-642-73790-9.
- Artini PG, Genazzani AR, Petraglia F (11 December 2001). Advances in Gynecological Endocrinology. CRC Press. pp. 105–. ISBN 978-1-84214-071-0.
- King TL, Brucker MC, Kriebs JM, Fahey JO (21 October 2013). Varney's Midwifery. Jones & Bartlett Publishers. pp. 495–. ISBN 978-1-284-02542-2.
- Ayub M, Levell MJ (August 1989). "The effect of ketoconazole related imidazole drugs and antiandrogens on [3H] R 1881 binding to the prostatic androgen receptor and [3H]5 alpha-dihydrotestosterone and [3H]cortisol binding to plasma proteins". J. Steroid Biochem. 33 (2): 251–5. doi:10.1016/0022-4731(89)90301-4. PMID 2788775.
- Pratt WB (1994). The Anticancer Drugs. Oxford University Press. pp. 219–. ISBN 978-0-19-506739-2.
- Plewig G, Kligman AM (6 December 2012). ACNE and ROSACEA. Springer Science & Business Media. pp. 662, 685. ISBN 978-3-642-59715-2.
- Kuhl H (2011). "Pharmacology of Progestogens" (PDF). J Reproduktionsmed Endokrinol. 8 (1): 157–177.
- Schneider HP (November 2003). "Androgens and antiandrogens". Ann. N. Y. Acad. Sci. 997 (1): 292–306. Bibcode:2003NYASA.997..292S. doi:10.1196/annals.1290.033. PMID 14644837. S2CID 8400556.
- Schröder FH (December 1993). "Cyproterone acetate--mechanism of action and clinical effectiveness in prostate cancer treatment". Cancer. 72 (12 Suppl): 3810–5. doi:10.1002/1097-0142(19931215)72:12+<3810::AID-CNCR2820721710>3.0.CO;2-O. PMID 8252496.
- Liang T, Rasmusson GH, Brooks JR (July 1983). "12. Androgens: Pharmacodynamics and antagonists. Biochemical and biological studies with 4-aza-steroidal 5 alpha-reductase inhibitors". J. Steroid Biochem. 19 (1A): 385–90. doi:10.1016/s0022-4731(83)80051-x. PMID 6887871.
- Eil C, Edelson SK (July 1984). "The use of human skin fibroblasts to obtain potency estimates of drug binding to androgen receptors". J. Clin. Endocrinol. Metab. 59 (1): 51–5. doi:10.1210/jcem-59-1-51. PMID 6725525.
- Brown TR, Rothwell SW, Sultan C, Migeon CJ (June 1981). "Inhibition of androgen binding in human foreskin fibroblasts by antiandrogens". Steroids. 37 (6): 635–48. doi:10.1016/S0039-128X(81)90173-2. PMID 6457421. S2CID 88959.
- Breiner M, Romalo G, Schweikert HU (August 1986). "Inhibition of androgen receptor binding by natural and synthetic steroids in cultured human genital skin fibroblasts". Klinische Wochenschrift. 64 (16): 732–7. doi:10.1007/BF01734339. PMID 3762019. S2CID 34846760.
- Breiner M, Romalo G, Schweikert HU (1986). "Inhibition of androgen receptor binding by drugs in cultured human genital skin fibroblasts". Acta Endocrinologica. 113 (1_Suppl): S152. doi:10.1530/acta.0.111S152. ISSN 0804-4643.
- Pharmacology of the Skin II: Methods, Absorption, Metabolism and Toxicity, Drugs and Diseases. Springer Science & Business Media. 6 December 2012. pp. 474, 489. ISBN 978-3-642-74054-1.
- Pucci E, Petraglia F (December 1997). "Treatment of androgen excess in females: yesterday, today and tomorrow". Gynecol. Endocrinol. 11 (6): 411–33. doi:10.3109/09513599709152569. PMID 9476091.
- Gräf KJ, Brotherton J, Neumann F (1974). "Clinical Uses of Antiandrogens". Androgens II and Antiandrogens / Androgene II und Antiandrogene. pp. 485–542. doi:10.1007/978-3-642-80859-3_7. ISBN 978-3-642-80861-6.
- Marsden JR, Shuster S (1989). "The Treatment of Acne". In Malcolm Greaves MW, Shuster S (eds.). Pharmacology of the Skin II. Handbook of Experimental Pharmacology. 87/2. pp. 473–481. doi:10.1007/978-3-642-74054-1_35. ISBN 978-3-642-74056-5.
- Thomson DS (1989). "Pharmacology of Anti-androgens in the Skin". Pharmacology of the Skin II. Handbook of Experimental Pharmacology. 87 / 2. pp. 483–493. doi:10.1007/978-3-642-74054-1_36. ISBN 978-3-642-74056-5. ISSN 0171-2004.
- Ward A, Brogden RN, Heel RC, Speight TM, Avery GS (July 1984). "Isotretinoin. A review of its pharmacological properties and therapeutic efficacy in acne and other skin disorders". Drugs. 28 (1): 6–37. doi:10.2165/00003495-198428010-00002. PMID 6235105.
- Cormane, R. H.; van der Meeren, H. L. M. (1981). "Cyproteronacetate in the management of severe acne in males". Archives of Dermatological Research. 271 (2): 183–187. doi:10.1007/BF00412545. ISSN 0340-3696. S2CID 12153042.
- Misch, K.J.; Dolman, W.F.G.; Neild, V.; Rhodes, E.L. (1986). "Response of Male Acne to Antiandrogen Therapy with Cyproterone Acetate". Dermatology. 173 (3): 139–142. doi:10.1159/000249236. ISSN 1018-8665. PMID 2945742.
- van Wayjen RG, van den Ende A (1971). "Clinical-pharmacological investigation of cyproterone acetate". Gynecol Invest. 2 (1): 282–9. doi:10.1159/000301868. PMID 5161488.
- Sitruk-Ware R (April 2004). "Pharmacological profile of progestins". Maturitas. 47 (4): 277–83. doi:10.1016/j.maturitas.2004.01.001. PMID 15063480.
- Becker KL (2001). Principles and Practice of Endocrinology and Metabolism. Lippincott Williams & Wilkins. pp. 1152–. ISBN 978-0-7817-1750-2.
- Kuhl H (April 2004). "Mechanisms of sex steroids. Future developments". Maturitas. 47 (4): 285–91. doi:10.1016/j.maturitas.2003.11.010. PMID 15063481.
- Miller JA, Jacobs HS (May 1986). "Treatment of hirsutism and acne with cyproterone acetate". Clin Endocrinol Metab. 15 (2): 373–89. doi:10.1016/S0300-595X(86)80031-7. PMID 2941191.
- Neumann, F; Jacobi, GH (March 1982). "Antiandrogens in tumour therapy". Clinics in Oncology. 1. pp. 41–64.
- Jacobi, G; Neumann, F (November 1988). "The Case for Cyproterone Acetate". Baillière's Clinical Oncology: International Practice and Research. 2 (3): 571–580. ISSN 0950-3560.
- Newling DW (March 1997). "The palliative therapy of advanced prostate cancer, with particular reference to the results of recent European clinical trials". Br J Urol. 79 Suppl 1: 72–81. doi:10.1111/j.1464-410X.1997.tb00805.x. PMID 9088277.
- Tunn, UW; Graff, J; Senge, Th (June 1982). "Treatment of inoperable prostatic cancer with cyproterone acetate". In Schröder, FH (ed.). Proceedings Androgens and Anti-androgens, International Symposium, Utrecht, June 5th, 1982. Schering Nederland BV. pp. 149–159. ISBN 978-9090004327. OCLC 11786945.
- Neumann, Friedmund (1996). "Pharmacology of Cyproterone Acetate — A Short Review". Antiandrogens in Prostate Cancer. pp. 31–44. doi:10.1007/978-3-642-45745-6_3. ISBN 978-3-642-45747-0.
- Meriggiola MC, Bremner WJ (1997). "Progestin-androgen combination regimens for male contraception". J. Androl. 18 (3): 240–4. doi:10.1002/j.1939-4640.1997.tb01913.x (inactive 17 January 2021). PMID 9203050.CS1 maint: DOI inactive as of January 2021 (link)
- Meriggiola MC, Costantino A, Bremner WJ, Morselli-Labate AM (2002). "Higher testosterone dose impairs sperm suppression induced by a combined androgen-progestin regimen". J. Androl. 23 (5): 684–90. doi:10.1002/j.1939-4640.2002.tb02311.x (inactive 17 January 2021). PMID 12185103.CS1 maint: DOI inactive as of January 2021 (link)
- Laschet U, Laschet L (June 1975). "Antiandrogens in the treatment of sexual deviations of men". J. Steroid Biochem. 6 (6): 821–6. doi:10.1016/0022-4731(75)90310-6. PMID 1177426.
- Labrie F (December 1993). "Mechanism of action and pure antiandrogenic properties of flutamide". Cancer. 72 (12 Suppl): 3816–27. doi:10.1002/1097-0142(19931215)72:12+<3816::AID-CNCR2820721711>3.0.CO;2-3. PMID 8252497.
- Simental JA, Sar M, Wilson EM (September 1992). "Domain functions of the androgen receptor". The Journal of Steroid Biochemistry and Molecular Biology. 43 (1–3): 37–41. doi:10.1016/0960-0760(92)90185-L. PMID 1525065. S2CID 43177646.
- Luthy IA, Begin DJ, Labrie F (November 1988). "Androgenic activity of synthetic progestins and spironolactone in androgen-sensitive mouse mammary carcinoma (Shionogi) cells in culture". Journal of Steroid Biochemistry. 31 (5): 845–52. doi:10.1016/0022-4731(88)90295-6. PMID 2462135.
- Térouanne B, Tahiri B, Georget V, Belon C, Poujol N, Avances C, Orio F, Balaguer P, Sultan C (February 2000). "A stable prostatic bioluminescent cell line to investigate androgen and antiandrogen effects". Molecular and Cellular Endocrinology. 160 (1–2): 39–49. doi:10.1016/s0303-7207(99)00251-8. PMID 10715537. S2CID 13737435.
- Fritz MA, Speroff L (20 December 2010). Clinical Gynecologic Endocrinology and Infertility. Lippincott Williams & Wilkins. p. 80. ISBN 978-0-7817-7968-5. Retrieved 27 May 2012.
- Schneider HP (December 2000). "The role of antiandrogens in hormone replacement therapy". Climacteric. 3 Suppl 2: 21–7. PMID 11379383.
- Poyet, Patrick; Labrie, Fernand (1985). "Comparison of the antiandrogenic/androgenic activities of flutamide, cyproterone acetate and megestrol acetate". Molecular and Cellular Endocrinology. 42 (3): 283–288. doi:10.1016/0303-7207(85)90059-0. ISSN 0303-7207. PMID 3930312. S2CID 24746807.
- Kampel LJ (20 March 2012). Dx/Rx: Prostate Cancer: Prostate Cancer. Jones & Bartlett Publishers. p. 169. ISBN 978-1-4496-8695-6.
- Singh SM, Gauthier S, Labrie F (February 2000). "Androgen receptor antagonists (antiandrogens): structure-activity relationships". Current Medicinal Chemistry. 7 (2): 211–47. doi:10.2174/0929867003375371. PMID 10637363.
When compared to flutamide, [cyproterone acetate] has significant intrinsic androgenic and estrogenic activities. [...] The effects of flutamide and the steroidal derivatives, cyproterone acetate, chlormadinone acetate, megestrol acetate and medroxyprogesterone acetate were compared in vivo in female nude mice bearing androgen-sensitive Shionogi tumors. All steroidal compounds stimulated tumor growth while flutamide had no stimulatory effect [51]. Thus, CPA due to its intrinsic properties stimulates androgen-sensitive parameters and cancer growth. Cyproterone acetate added to castration has never been shown in any controlled study to prolong disease-free survival or overall survival in prostate cancer when compared with castration alone [152-155].
- El Etreby, M. Fathy; Habenicht, Ursula-F.; Louton, Thomas; Nishino, Yukishige; Schröder, Helmut G. (1987). "Effect of cyproterone acetate in comparison to flutamide and megestrol acetate on the ventral prostate, seminal vesicle, and adrenal glands of adult male rats". The Prostate. 11 (4): 361–375. doi:10.1002/pros.2990110408. ISSN 0270-4137. PMID 2960960. S2CID 86447179.
- Habenicht, U.-F.; Düsterberg, B.; El Etreby, M. F.; Neumann, F. (1985). "Does cyproterone acetate have an androgen agonistic effect?". Acta Endocrinologica. 110 (1_Suppla): S152–S153. doi:10.1530/acta.0.109S152-a. ISSN 0804-4643.
- Schröder, Fritz H.; Radlmaier, Albert (2009). "Steroidal Antiandrogens". In V. Craig Jordan; Barrington J. A. Furr (eds.). Hormone Therapy in Breast and Prostate Cancer. Humana Press. pp. 325–346. doi:10.1007/978-1-59259-152-7_15. ISBN 978-1-60761-471-5.
- Vincens M, Mercier-Bodard C, Mowszowicz I, Kuttenn F, Mauvais-Jarvis P (October 1989). "Testosterone-estradiol binding globulin (TeBG) in hirsute patients treated with cyproterone acetate (CPA) and percutaneous estradiol". J. Steroid Biochem. 33 (4A): 531–4. doi:10.1016/0022-4731(89)90037-x. PMID 2530403.
- Elger, W. (1995). Pharmacology of antiandrogens and their clinical application. Current Science, 68(4), 459–469. https://www.jstor.org/stable/24096450
- Khalil R, Antonio L, Laurent MR, David K, Kim NR, Evenepoel P, Eisenhauer A, Heuser A, Cavalier E, Khosla S, Claessens F, Vanderschueren D, Decallonne B (August 2020). "Early effects of androgen deprivation on bone and mineral homeostasis in adult men: a prospective cohort study". Eur J Endocrinol. 183 (2): 181–189. doi:10.1530/EJE-20-0348. PMID 32454455.
- Godsland IF, Wynn V, Crook D, Miller NE (December 1987). "Sex, plasma lipoproteins, and atherosclerosis: prevailing assumptions and outstanding questions". Am. Heart J. 114 (6): 1467–503. doi:10.1016/0002-8703(87)90552-7. PMID 3318361.
- Lax ER (1987). "Mechanisms of physiological and pharmacological sex hormone action on the mammalian liver". J. Steroid Biochem. 27 (4–6): 1119–28. doi:10.1016/0022-4731(87)90198-1. PMID 3320549.
- Lax ER, Baumann P, Schriefers H (August 1983). "Antiandrogenic effects of oestradiol on enzyme activities of hepatic steroid metabolism". Exp. Clin. Endocrinol. 82 (2): 145–52. doi:10.1055/s-0029-1210270. PMID 6578932.
- Miyamoto, Hiroshi; Rahman, Mujib M.; Chang, Chawnshang (2004). "Molecular basis for the antiandrogen withdrawal syndrome". Journal of Cellular Biochemistry. 91 (1): 3–12. doi:10.1002/jcb.10757. ISSN 0730-2312. PMID 14689576. S2CID 5773128.
- Paul, Roger; Breul, Juergen (2000). "Antiandrogen Withdrawal Syndrome Associated with Prostate Cancer Therapies: Incidence and Clinical Significance". Drug Safety. 23 (5): 381–390. doi:10.2165/00002018-200023050-00003. ISSN 0114-5916. PMID 11085345. S2CID 7402525.
- Sella, A.; Flex, D.; Sulkes, A.; Baniel, J. (1998). "Antiandrogen withdrawal syndrome with cyproterone acetate". Urology. 52 (6): 1091–1093. doi:10.1016/S0090-4295(98)00354-9. ISSN 0090-4295. PMID 9836560.
- Rabe T, Kowald A, Ortmann J, Rehberger-Schneider S (August 2000). "Inhibition of skin 5 alpha-reductase by oral contraceptive progestins in vitro". Gynecological Endocrinology. 14 (4): 223–30. doi:10.3109/09513590009167685. PMID 11075290. S2CID 72220210.
- Stárka L, Sulcová J, Broulík P (1976). "Effect of cyproterone acetate on the action and metabolism of testosterone in the mouse kidney". Endokrinologie. 68 (2): 155–63. PMID 1009901.
- Raudrant D, Rabe T (2003). "Progestogens with antiandrogenic properties". Drugs. 63 (5): 463–92. doi:10.2165/00003495-200363050-00003. PMID 12600226. S2CID 28436828.
- Neumann F, Steinbeck H (1974). "Antiandrogens". Androgens II and Antiandrogens / Androgene II und Antiandrogene. pp. 235–484. doi:10.1007/978-3-642-80859-3_6. ISBN 978-3-642-80861-6.
- Tartagni M, Schonauer LM, De Salvia MA, Cicinelli E, De Pergola G, D'Addario V (April 2000). "Comparison of Diane 35 and Diane 35 plus finasteride in the treatment of hirsutism". Fertility and Sterility. 73 (4): 718–23. doi:10.1016/s0015-0282(99)00633-0. PMID 10731531.
- Sahin Y, Dilber S, Keleştimur F (March 2001). "Comparison of Diane 35 and Diane 35 plus finasteride in the treatment of hirsutism". Fertility and Sterility. 75 (3): 496–500. doi:10.1016/s0015-0282(00)01764-7. PMID 11239530.
- Fritz MA, Speroff L (2011). Clinical Gynecologic Endocrinology and Infertility. Lippincott Williams & Wilkins. pp. 561–. ISBN 978-0-7817-7968-5.
- Reed MJ, Franks S (September 1988). "Anti-androgens in gynaecological practice". Baillière's Clin Obstet Gynaecol. 2 (3): 581–95. doi:10.1016/S0950-3552(88)80045-2. PMID 2976627.
- Hammerstein, J (1979). "Cyproterone acetate". Advances in Gynaecological Endocrinology: Proceedings of the Sixth Study Group of the Royal College of Obstetricians and Gynaecologists, 18th and 19th October, 1978. The College. pp. 367–368, 374. ISBN 978-0-87489-225-3.
CPA may be characterized endocrinologically as possessing strong progestational, moderate anti-androgenic and limited anti-gonadotropic potencies. [...] Its progestational activity, in terms of the transformation dose in the oestrogen-primed human endometrium, is 20–30 mg which is comparable to that of chlormadinone acetate and other strong progestogens (Table I). To take full clinical advantage of its anti-androgenicity not less than 50–100 mg CPA must be taken orally per day, which totals 2 to 3 times the progestational activity the female organism is exposed to throughout a complete ovulatory menstrual cycle. Thus unless much lower and less efficacious doses of CPA are used, a tremendous progestational overdosage must be accepted. [...] As already pointed out CPA is endocrinologically not a well-balanced compound because of the strong preponderance of the progestational over the anti-androgenic potency. A way to avoid the heavy progestogen overdosage inherent with the high-dose reverse sequential therapy would be to combine the low-dose contraceptive formulation just mentioned with a pure anti-androgen such as free cyproterone (Table 2).
- Hammerstein J, Meckies J, Leo-Rossberg I, Moltz L, Zielske F (June 1975). "Use of cyproterone acetate (CPA) in the treatment of acne, hirsutism and virilism". J. Steroid Biochem. 6 (6): 827–36. doi:10.1016/0022-4731(75)90311-8. PMID 126335.
- Herbert DC, Schuppler J, Poggel A, Günzel P, El Etreby MF (1977). "Effect of cyproterone acetate on prolactin secretion in the female Rhesus monkey". Cell Tissue Res. 183 (1): 51–60. doi:10.1007/bf00219991. PMID 411573. S2CID 25943599.
- Kanhai RC, Hage JJ, van Diest PJ, Bloemena E, Mulder JW (January 2000). "Short-term and long-term histologic effects of castration and estrogen treatment on breast tissue of 14 male-to-female transsexuals in comparison with two chemically castrated men". The American Journal of Surgical Pathology. 24 (1): 74–80. doi:10.1097/00000478-200001000-00009. PMID 10632490.
- Lawrence, Anne A. (2007). "Transgender Health Concerns". The Health of Sexual Minorities. pp. 473–505. doi:10.1007/978-0-387-31334-4_19. ISBN 978-0-387-28871-0. Missing or empty
|title=(help) - Rosen PP (2009). Rosen's Breast Pathology. Lippincott Williams & Wilkins. pp. 31–. ISBN 978-0-7817-7137-5.
- Lorincz AM, Sukumar S (2006). "Molecular links between obesity and breast cancer". Endocrine-Related Cancer. 13 (2): 279–92. doi:10.1677/erc.1.00729. PMID 16728564.
Adipocytes make up the bulk of the human breast, with epithelial cells accounting for only approximately 10% of human breast volume.
- Howard BA, Gusterson BA (2000). "Human breast development". Journal of Mammary Gland Biology and Neoplasia. 5 (2): 119–37. doi:10.1023/a:1026487120779. PMID 11149569. S2CID 10819224.
In the stroma, there is an increase in the amount of fibrous and fatty tissue, with the adult nonlactating breast consisting of 80% or more of stroma.
- Sperling MA (10 April 2014). Pediatric Endocrinology. Elsevier Health Sciences. pp. 598–. ISBN 978-1-4557-5973-6.
Estrogen stimulates the nipples to grow, mammary terminal duct branching to progress to the stage at which ductules are formed, and fatty stromal growth to increase until it constitutes about 85% of the mass of the breast. [...] Lobulation appears around menarche, when multiple blind saccular buds form by branching of the terminal ducts. These effects are due to the presence of progesterone. [...] Full alveolar development normally only occurs during pregnancy under the influence of additional progesterone and prolactin.
- Hagisawa S, Shimura N, Arisaka O (2012). "Effect of excess estrogen on breast and external genitalia development in growth hormone deficiency". Journal of Pediatric and Adolescent Gynecology. 25 (3): e61–3. doi:10.1016/j.jpag.2011.11.005. PMID 22206682.
Estrogen stimulates growth of the nipples, progression of mammary duct branching to the stage at which ductiles are formed, and fatty stromal growth until it constitutes about 85% of the mass of the breast.
- Wierckx K, Gooren L, T'Sjoen G (May 2014). "Clinical review: Breast development in trans women receiving cross-sex hormones". The Journal of Sexual Medicine. 11 (5): 1240–7. doi:10.1111/jsm.12487. PMID 24618412.
- Nota NM, Dekker MJ, Klaver M, Wiepjes CM, van Trotsenburg MA, Heijboer AC, den Heijer M (August 2017). "Prolactin levels during short- and long-term cross-sex hormone treatment: an observational study in transgender persons". Andrologia. 49 (6): e12666. doi:10.1111/and.12666. PMID 27561756. S2CID 25268468.
- Iversen P, Melezinek I, Schmidt A (January 2001). "Nonsteroidal antiandrogens: a therapeutic option for patients with advanced prostate cancer who wish to retain sexual interest and function". BJU International. 87 (1): 47–56. doi:10.1046/j.1464-410x.2001.00988.x. PMID 11121992. S2CID 28215804.
- Donald RA, Espiner EA, Cowles RJ, Fazackerley JE (April 1976). "The effect of cyproterone acetate on the plasma gonadotrophin response to gonadotrophin releasing hormone". Acta Endocrinologica. 81 (4): 680–4. doi:10.1530/acta.0.0810680. PMID 769466.
- Moltz L, Römmler A, Post K, Schwartz U, Hammerstein J (April 1980). "Medium dose cyproterone acetate (CPA): effects on hormone secretion and on spermatogenesis in men". Contraception. 21 (4): 393–413. doi:10.1016/s0010-7824(80)80017-5. PMID 6771095.
- Rost A, Schmidt-Gollwitzer M, Hantelmann W, Brosig W (1981). "Cyproterone acetate, testosterone, LH, FSH, and prolactin levels in plasma after intramuscular application of cyproterone acetate in patients with prostatic cancer". The Prostate. 2 (3): 315–22. doi:10.1002/pros.2990020310. PMID 6458025. S2CID 22364184.
- Jeffcoate WJ, Matthews RW, Edwards CR, Field LH, Besser GM (August 1980). "The effect of cyproterone acetate on serum testosterone, LH, FSH, and prolactin in male sexual offenders". Clinical Endocrinology. 13 (2): 189–95. doi:10.1111/j.1365-2265.1980.tb01041.x. PMID 6777092. S2CID 10145079.
- Grunwald K, Rabe T, Schlereth G, Runnebaum B (November 1994). "[Serum hormones before and during therapy with cyproterone acetate and spironolactone in patients with androgenization]". Geburtshilfe und Frauenheilkunde (in German). 54 (11): 634–45. doi:10.1055/s-2007-1022355. PMID 8719011.
- Salva P, Morer F, Ordoñez J, Rodriguez J (1983). "Treatment of idiopathic hirsute women with two combinations of cyproterone acetate". International Journal of Clinical Pharmacology Research. 3 (2): 129–35. PMID 6237068.
- Payne AH, Hardy MP (28 October 2007). The Leydig Cell in Health and Disease. Springer Science & Business Media. pp. 426–. ISBN 978-1-59745-453-7.
- Nieschlag E, Habenicht UF (17 April 2013). Spermatogenesis — Fertilization — Contraception: Molecular, Cellular and Endocrine Events in Male Reproduction. Springer Science & Business Media. pp. 485–. ISBN 978-3-662-02815-5.
- Wu FC (October 1988). "Male contraception: current status and future prospects". Clin. Endocrinol. (Oxf). 29 (4): 443–65. doi:10.1111/j.1365-2265.1988.tb02894.x. PMID 3075164. S2CID 36608203.
Cyproterone acetate (CPA) is an antiandrogen with progestational effects. It was originally intended as an antifertility agent through its antiandrogen action on the epididymis (Prasad et al., 1970). However, it subsequently became clear that CPA acted as a gestagen to suppress gonadotrophins and testosterone even at the low doses of 5 to 10 mg daily (Wang & Yeung, 1980).
- Koch UJ, Lorenz F, Danehl K, Ericsson R, Hasan SH, Keyserlingk DV, Lübke K, Mehring M, Römmler A, Schwartz U, Hammerstein J (August 1976). "Continuous oral low-dosage cyproterone acetate for fertility regulation in the male? A trend analysis in 15 volunteers". Contraception. 14 (2): 117–35. doi:10.1016/0010-7824(76)90081-0. PMID 949890.
- Wang C, Yeung KK (March 1980). "Use of low-dosage oral cyproterone acetate as a male contraceptive". Contraception. 21 (3): 245–72. doi:10.1016/0010-7824(80)90005-0. PMID 6771091.
- Jacobi GH, Altwein JE, Kurth KH, Basting R, Hohenfellner R (1980). "Treatment of advanced prostatic cancer with parenteral cyproterone acetate: a phase III randomised trial". Br J Urol. 52 (3): 208–15. doi:10.1111/j.1464-410x.1980.tb02961.x. PMID 7000222.
- Knuth UA, Hano R, Nieschlag E (November 1984). "Effect of flutamide or cyproterone acetate on pituitary and testicular hormones in normal men". The Journal of Clinical Endocrinology and Metabolism. 59 (5): 963–9. doi:10.1210/jcem-59-5-963. PMID 6237116.
- Gijs, Luk; Gooren, Louis (1996). "Hormonal and psychopharmacological interventions in the treatment of paraphilias: An update". Journal of Sex Research. 33 (4): 273–290. doi:10.1080/00224499609551845. ISSN 0022-4499.
Some researchers have recommended never stopping medication, but continuing the use of 12.5 to 25 mg CPA a day as a maintenance dose (Bradford & Pawlak, 1993a).
- Bradford, John M. W.; Pawlak, Anne (1993). "Double-blind placebo crossover study of cyproterone acetate in the treatment of the paraphilias". Archives of Sexual Behavior. 22 (5): 383–402. doi:10.1007/BF01542555. ISSN 0004-0002. PMID 8239971. S2CID 9472016.
A number of individuals (not included in this study), who have been on CPA for longer periods and then remained on very low dosages of CPA (12.5 to 25 mg per day), have reported no recurrence of the deviant sexual fantasies and no paraphiliac behavior ever reoccurred. Some of these individuals have remained in treatment for a number of years without any further paraphilic behavior.
- Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA (25 August 2011). Campbell-Walsh Urology: Expert Consult Premium Edition: Enhanced Online Features and Print, 4-Volume Set. Elsevier Health Sciences. pp. 2938–. ISBN 978-1-4160-6911-9.
- Wenderoth UK, Jacobi GH (1983). "Gonadotropin-releasing hormone analogues for palliation of carcinoma of the prostate". World Journal of Urology. 1 (1): 40–48. doi:10.1007/BF00326861. ISSN 0724-4983. S2CID 23447326.
- Fourcade RO, McLeod D (2015). "Tolerability of Antiandrogens in the Treatment of Prostate Cancer". UroOncology. 4 (1): 5–13. doi:10.1080/1561095042000191655. ISSN 1561-0950.
- D’Agata, R.; Gulizia, S.; Vicari, E.; Aliffi, A.; Polosa, P. (1979). "Effect of Cyproterone Acetate Acutely Administered on the Pituitary-Testicular Axis". Hormone Research. 11 (3): 109–114. doi:10.1159/000179046. ISSN 1423-0046. PMID 488903.CS1 maint: multiple names: authors list (link)
- Saborowski, Karl-Johannes (1988), Konservative Therapie mit Cyproteronacetat und Estradiolundecylat beim Fortgeschrittenen Prostatacarcinom: Eine 5-Jahres-Studie [Conservative Therapy with Cyproterone Acetate and Estradiol Undecylate in Advanced Prostate Cancer: A 5-Year Study] (in German), Bochum, Univ., Diss., OCLC 917571781
- Melamed AJ (March 1987). "Current concepts in the treatment of prostate cancer". Drug Intell Clin Pharm. 21 (3): 247–54. doi:10.1177/106002808702100302. PMID 3552544. S2CID 7482144.
[Megestrol acetate] produces a transient reduction in plasma testosterone to levels somewhat higher than those in castrated men. When used in a dose of 40 mg tid, in combination with estradiol 0.5–1.5 mg/d, it acts synergistically to suppress pituitary gonadotropins and maintain plasma testosterone at castration levels for periods up to one year.
- Tangpricha V, den Heijer M (April 2017). "Oestrogen and anti-androgen therapy for transgender women". Lancet Diabetes Endocrinol. 5 (4): 291–300. doi:10.1016/S2213-8587(16)30319-9. PMC 5366074. PMID 27916515.
- Fung R, Hellstern-Layefsky M, Lega I (2017). "Is a lower dose of cyproterone acetate as effective at testosterone suppression in transgender women as higher doses?". International Journal of Transgenderism. 18 (2): 123–128. doi:10.1080/15532739.2017.1290566. ISSN 1553-2739. S2CID 79095497.
- Cheung AS, Ooi O, Davidoff D, Leemaqz SY, Cundill P, Silberstein N, Bretherton I, Grossmann M, Zajac JD (2018). "Cyproterone vs spironolactone as anti‐androgen therapy for transgender females receiving oestradiol therapy". Clinical Endocrinology. 89: 4–94. doi:10.1111/cen.13727. ISSN 0300-0664. PMID 29952008.
- Goldenberg SL, Bruchovsky N, Rennie PS, Coppin CM (December 1988). "The combination of cyproterone acetate and low dose diethylstilbestrol in the treatment of advanced prostatic carcinoma". J. Urol. 140 (6): 1460–5. doi:10.1016/S0022-5347(17)42073-8. PMID 2973529.
- Goldenberg SL, Bruchovsky N, Gleave ME, Sullivan LD (June 1996). "Low-dose cyproterone acetate plus mini-dose diethylstilbestrol--a protocol for reversible medical castration". Urology. 47 (6): 882–4. doi:10.1016/S0090-4295(96)00048-9. PMID 8677581.
- Bruchovsky N, Goldenberg SL, Akakura K, Rennie PS (September 1993). "Luteinizing hormone-releasing hormone agonists in prostate cancer. Elimination of flare reaction by pretreatment with cyproterone acetate and low-dose diethylstilbestrol". Cancer. 72 (5): 1685–91. doi:10.1002/1097-0142(19930901)72:5<1685::AID-CNCR2820720532>3.0.CO;2-3. PMID 7688656.
- Meriggiola MC, Bremner WJ, Costantino A, Bertaccini A, Morselli-Labate AM, Huebler D, Kaufmann G, Oettel M, Flamigni C (May 2002). "Twenty-one day administration of dienogest reversibly suppresses gonadotropins and testosterone in normal men". J. Clin. Endocrinol. Metab. 87 (5): 2107–13. doi:10.1210/jcem.87.5.8514. hdl:1773/4465. PMID 11994349.
- Moltz L, Römmler A, Schwartz U, Post K, Hammerstein J (1978). "252. Cyproterone acetate (CPA)-a potential male contraceptive: further studies on the interactions with endocrine parameters". Journal of Steroid Biochemistry. 9 (9): 865. doi:10.1016/0022-4731(78)90952-4. ISSN 0022-4731.
- Moltz L, Römmler A, Schwartz U, Hammerstein J (1978). "Effects of Cyproterone Acetate (CPA) on Pituitary Gonadotrophin Release and on Androgen Secretion Before and After LH-RH Double Stimulation Tests in Men". International Journal of Andrology. 1 (s2b): 713–719. doi:10.1111/j.1365-2605.1978.tb00518.x. ISSN 0105-6263.
- Koch UJ, Lorenz F, Danehl K, Hammerstein J (November 1975). "Über die Verwendbarkeit von Cyproteronacetat zur Fertilitätshemmung beim Mann. Morphologische Veränderungen und Einflüsse auf die Spermienmotilität" [Use of cyproterone acetate for fertility inhibition in the male. Morphologic changes and influences on sperm motility]. Arch Gynakol (in German). 219 (1–4): 581–2. doi:10.1007/BF00669258. PMID 1243497.
- Gava, Giulia; Cerpolini, Silvia; Martelli, Valentina; Battista, Giuseppe; Seracchioli, Renato; Meriggiola, Maria Cristina (2016). "Cyproterone acetate vs leuprolide acetate in combination with transdermal oestradiol in transwomen: a comparison of safety and effectiveness". Clinical Endocrinology. 85 (2): 239–246. doi:10.1111/cen.13050. ISSN 0300-0664.
- Angus L, Leemaqz S, Ooi O, Cundill P, Silberstein N, Locke P, Zajac JD, Cheung AS (July 2019). "Cyproterone acetate or spironolactone in lowering testosterone concentrations for transgender individuals receiving oestradiol therapy". Endocr Connect. 8 (7): 935–940. doi:10.1530/EC-19-0272. PMC 6612061. PMID 31234145.
- Eden JA (December 1991). "Progestogens: an occasional review". Asia Oceania J Obstet Gynaecol. 17 (4): 289–95. doi:10.1111/j.1447-0756.1991.tb00276.x. PMID 1801674.
CPA is a progestogen which is anti-oestrogenic but also antiandrogenic and in high doses (higher than 100 mg) has mild glucocorticoid actions.
- Bhargava AS, Kapp JF, Poggel HA, Heinick J, Nieuweboer B, Günzel P (1981). "Effect of cyproterone acetate and its metabolites on the adrenal function in man, rhesus monkey and rat". Arzneimittelforschung. 31 (6): 1005–9. PMID 6266428.
- van Wayjen RG, van den Ende A (1981). "Effect of cyproterone acetate on pituitary-adrenocortical function in man". Acta Endocrinol. 96 (1): 112–22. doi:10.1530/acta.0.0960112. PMID 6257015.
- Schürmeyer T, Graff J, Senge T, Nieschlag E (1986). "Effect of oestrogen or cyproterone acetate treatment on adrenocortical function in prostate carcinoma patients". Acta Endocrinol. 111 (3): 360–7. doi:10.1530/acta.0.1110360. PMID 2421511.
- van Wayjen RG, van den Ende A (1995). "Experience in the long-term treatment of patients with hirsutism and/or acne with cyproterone acetate-containing preparations: efficacy, metabolic and endocrine effects". Exp. Clin. Endocrinol. Diabetes. 103 (4): 241–51. doi:10.1055/s-0029-1211357. PMID 7584530.
- Holdaway IM, Croxson MS, Evans MC, France J, Sheehan A, Wilson T, Ibbertson HK (1983). "Effect of cyproterone acetate on glucocorticoid secretion in patients treated for hirsutism". Acta Endocrinol. 104 (2): 222–6. doi:10.1530/acta.0.1040222. PMID 6227191.
- Azziz R (8 November 2007). Androgen Excess Disorders in Women. Springer Science & Business Media. pp. 382–. ISBN 978-1-59745-179-6.
- Girard J, Baumann JB, Bühler U, Zuppinger K, Haas HG, Staub JJ, Wyss HI (1978). "Cyproteroneacetate and ACTH adrenal function". J. Clin. Endocrinol. Metab. 47 (3): 581–6. doi:10.1210/jcem-47-3-581. PMID 233676.
- Panesar NS, Herries DG, Stitch SR (1979). "Effects of cyproterone and cyproterone acetate on the adrenal gland in the rat: studies in vivo and in vitro". J. Endocrinol. 80 (2): 229–38. doi:10.1677/joe.0.0800229. PMID 438696.
- El Etreby MF (1979). "Effect of cyproterone acetate, levonorgestrel and progesterone on adrenal glands and reproductive organs in the beagle bitch". Cell Tissue Res. 200 (2): 229–43. doi:10.1007/bf00236416. PMID 487397. S2CID 20443285.
- Savage DC, Swift PG (1981). "Effect of cyproterone acetate on adrenocortical function in children with precocious puberty". Arch. Dis. Child. 56 (3): 218–22. doi:10.1136/adc.56.3.218. PMC 1627152. PMID 6260040.
- Stivel MS, Kauli R, Kaufman H, Laron Z (1982). "Adrenocortical function in children with precocious sexual development during treatment with cyproterone acetate". Clin. Endocrinol. 16 (2): 163–9. doi:10.1111/j.1365-2265.1982.tb03160.x. PMID 6279337. S2CID 21454179.
- Hague WM, Munro DS, Sawers RS, Duncan SL, Honour JW (1982). "Long-term effects of cyproterone acetate on the pituitary adrenal axis in adult women". Br J Obstet Gynaecol. 89 (12): 981–4. doi:10.1111/j.1471-0528.1982.tb04650.x. PMID 6216913. S2CID 40574520.
- Mercier L, Miller PA, Simons SS (1986). "Antiglucocorticoid steroids have increased agonist activity in those hepatoma cell lines that are more sensitive to glucocorticoids". J. Steroid Biochem. 25 (1): 11–20. doi:10.1016/0022-4731(86)90275-x. PMID 2875214.
- Poulin R, Baker D, Poirier D, Labrie F (1991). "Multiple actions of synthetic 'progestins' on the growth of ZR-75-1 human breast cancer cells: an in vitro model for the simultaneous assay of androgen, progestin, estrogen, and glucocorticoid agonistic and antagonistic activities of steroids". Breast Cancer Research and Treatment. 17 (3): 197–210. doi:10.1007/BF01806369. PMID 1645605. S2CID 26083052.
- Pham-Huu-Trung MT, de Smitter N, Bogyo A, Girard F (1984). "Effects of cyproterone acetate on adrenal steroidogenesis in vitro". Horm. Res. 20 (2): 108–15. doi:10.1159/000179982. PMID 6237971.
- Lambert A, Mitchell RM, Robertson WR (1985). "On the site of action of the anti-adrenal steroidogenic effect of cyproterone acetate". Biochem. Pharmacol. 34 (12): 2091–5. doi:10.1016/0006-2952(85)90400-9. PMID 2988566.
- Heinze F, Teller WM, Fehm HL, Joos A (1978). "The effect of cyproterone acetate on adrenal cortical function in children with precocious puberty". Eur. J. Pediatr. 128 (2): 81–8. doi:10.1007/bf00496993. PMID 208851. S2CID 25215020.
- Bhargava AS, Seeger A, Günzel P (1977). "Isolation and identification of 15-beta-hydroxy cyproterone acetate as a new metabolite of cyproterone acetate in dog, monkey and man". Steroids. 30 (3): 407–18. doi:10.1016/0039-128x(77)90031-9. PMID 413211. S2CID 54373018.
- Broulik PD, Starka L (1975). "Corticosteroid-like effect of cyproterone and cyproterone acetate in mice". Experientia. 31 (11): 1364–5. doi:10.1007/bf01945829. PMID 1204803. S2CID 11452300.
- Thomas JA (12 March 1997). Endocrine Toxicology, Second Edition. CRC Press. pp. 152–. ISBN 978-1-4398-1048-4.
- Panay N (31 August 2015). Managing the Menopause. Cambridge University Press. pp. 126–. ISBN 978-1-107-45182-7.
- Luttge WG, Gray HE, Hughes JR (March 1976). "Regional and subcellular [3h]estradiol localization in selected brain regions and pituitary of female mice: effects of unlabeled estradiol and various anti-hormones". Brain Res. 104 (2): 273–81. doi:10.1016/0006-8993(76)90619-3. PMID 1260424. S2CID 10297027.
- Arya M, Lohiya NK (1977). "Estrogenic and antifertility effect of cyproterone acetate in female gerbils, meriones hurriane Jerdon". Acta Biol. Med. Ger. 36 (7–8): 1133–41. PMID 612093.
- Lohika NK, Arya M (June 1979). "Effect of cyproterone acetate on the genital organs of female rats". Acta Eur. Fertil. 10 (2): 57–65. PMID 94736.
- Lohiya NK, Arya M (October 1981). "Oestrogenic activity of cyproterone acetate in female mice". Endokrinologie. 78 (1): 21–7. PMID 6172270.
- Gutiérrez M, Menéndez L, Ruiz-Gayo M, Hidalgo A, Baamonde A (June 1997). "Cyproterone acetate displaces opiate binding in mouse brain". European Journal of Pharmacology. 328 (1): 99–102. doi:10.1016/s0014-2999(97)83034-8. PMID 9203575.
- Gruber CJ, Huber JC (December 2003). "Differential effects of progestins on the brain". Maturitas. 46 Suppl 1: S71–5. doi:10.1016/j.maturitas.2003.09.021. PMID 14670648.
- "Mylan-Cyproterone Label" (PDF).
- Saleh FM, Grudzinskas AJ, Bradford JM (11 February 2009). Sex Offenders: Identification, Risk Assessment, Treatment, and Legal Issues. Oxford University Press, USA. pp. 197–. ISBN 978-0-19-517704-6.
- Hümpel M, Wendt H, Schulze PE, Dogs G, Weiss C, Speck U (May 1977). "Bioavailability and pharmacokinetics of cyproterone acetate after oral administration of 2.0 mg cyproterone acetate in combination with 50 micrograms ethinyloestradiol to 6 young women". Contraception. 15 (5): 579–88. doi:10.1016/0010-7824(77)90108-1. PMID 880829.
- Hümpel M, Wendt H, Dogs G, Weiss C, Rietz S, Speck U (1977). "Intraindividual comparison of pharmacokinetic parameters of d-norgestrel, lynestrenol and cyproterone acetate in 6 women". Contraception. 16 (2): 199–215. doi:10.1016/0010-7824(77)90087-7. ISSN 0010-7824.
- Düsterberg B, Hümpel M, Wendt H (1979). "Plasma levels of active ingredients after single and repeated administration of a new oral contraceptive containing 2 mg of cyproterone acetate and 50 micrograms of ethinyl estradiol (DIANE) to five young women". Acta Obstet Gynecol Scand Suppl. 88: 27–31. doi:10.3109/00016347909157226. PMID 294111. S2CID 12805693.
- Kuhnz W, Staks T, Jütting G (December 1993). "Pharmacokinetics of cyproterone acetate and ethinylestradiol in 15 women who received a combination oral contraceptive during three treatment cycles". Contraception. 48 (6): 557–75. doi:10.1016/0010-7824(93)90118-Q. PMID 8131397.
- Kuhnz W, Kulmann H, Fuhrmeister A (1997). "Investigation into the age-dependence of the pharmacokinetics of cyproterone acetate in healthy male volunteers". Eur. J. Clin. Pharmacol. 53 (1): 75–80. doi:10.1007/s002280050340. PMID 9349934. S2CID 25219124.
- Ching, RCK (2006). Avaliação de bioquivalência de comprimidos contendo 100 mg de acetato de ciproterona (PDF) (PhD) (in Portuguese). Universidade de São Paulo.
- Frölich M, Vader HL, Walma ST, de Rooy HA (September 1980). "Cyproterone acetate in blood of hirsute women during long-term treatment. The absorption and elimination after oral application". J. Steroid Biochem. 13 (9): 1097–100. doi:10.1016/0022-4731(80)90142-9. PMID 7421247.
- Neumann, F; Hümpel, M; Senge, Th; Schenck, B; Tunn, U (1 December 1982). "Cyproterone Acetate—Biochemical and Biological Basis for Treatment of Prostatic Cancer". In Jacobi, Günther H; Hohenfellner, Rudolf (eds.). Prostate Cancer. Williams & Wilkins. pp. 269–303. ISBN 978-0-683-04354-9.
- Neumann F, Wiechert R (March 1988). "Das Antiandrogen Cyproteronacetat Seine Geschichte von der Entdeckung bis zur Marktreife" [The antiandrogen cyproterone acetate. Its history from discovery to marketing]. Pharmazie in Unserer Zeit (in German). 17 (2): 33–50. doi:10.1002/pauz.19880170202. ISSN 0048-3664. PMID 2967500.
- Hammerstein J, Moltz L, Schwartz U (July 1983). "Antiandrogens in the treatment of acne and hirsutism". J. Steroid Biochem. 19 (1B): 591–7. doi:10.1016/0022-4731(83)90223-6. PMID 6224974.
- Denmeade SR, Isaacs JT (May 2002). "A history of prostate cancer treatment". Nat. Rev. Cancer. 2 (5): 389–96. doi:10.1038/nrc801. PMC 4124639. PMID 12044015.
- Schindler AE (2015). "Pharmacology of Progestogens". In Carp HJ (ed.). Progestogens in Obstetrics and Gynecology. Springer. pp. 38–. ISBN 978-3-319-14385-9.
- Barra F, Scala C, Ferrero S (April 2018). "Current understanding on pharmacokinetics, clinical efficacy and safety of progestins for treating pain associated to endometriosis". Expert Opin Drug Metab Toxicol. 14 (4): 399–415. doi:10.1080/17425255.2018.1461840. hdl:11567/912822. PMID 29617576. S2CID 4731449.
- Rabe T, Albring C, Blume-Peytavi U, Egarter C, Geisthövel F, König K, Kuhl H, Merkle E, Mueck AO, Reisch N, Schüring A, Stute P, Toth B, Wildt L, Zouboulis CC (2015). "Hirsutismus – Medikamentöse Therapie Gemeinsame Stellungnahme der Deutschen Gesellschaft für Gynäkologische Endokrinologie und Fortpflanzungsmedizin e.V. und des Berufsverbands der Frauenärzte e.V." [Hirsutism – Medicinal treatment. Joint statement of the German Society of Gynaecological Endocrinology and Reproductive Medicine and the Professional Association of Gynaecologists]. Journal für Reproduktionsmedizin und Endokrinologie (in German). 12 (3): 102–149. ISSN 1810-2107.
- Fischl FH (2001). "Pharmacology of Estrogens and Gestagens" (PDF). In Krause & Pachemegg (ed.). Menopause andropause (PDF). Gablitz: Krause und Pachernegg. pp. 33–50. ISBN 978-3-901299-34-6.
- New Zealand Medicines; Medical Devices Safety Authority (9 December 2005). "Data Sheet: Diane 35 ED". Archived from the original on 8 January 2007.
- Medicines and Healthcare products Regulatory Authority (11 April 2006). "Cyproterone Acetate" (PDF). Archived from the original (PDF) on 28 September 2007. Retrieved 23 December 2018.
- Berlex Canada, Inc. (10 February 2003). "Cyproterone Acetate Tablets and Injections Product Monographs (revised version)" (PDF). Archived from the original (PDF) on 24 September 2006.
- Giorgi EP, Shirley IM, Grant JK, Stewart JC (March 1973). "Androgen dynamics in vitro in the human prostate gland. Effect of cyproterone and cyproterone acetate". The Biochemical Journal. 132 (3): 465–74. doi:10.1042/bj1320465. PMC 1177610. PMID 4125095.
- Anderson J (March 2003). "The role of antiandrogen monotherapy in the treatment of prostate cancer". BJU Int. 91 (5): 455–61. doi:10.1046/j.1464-410X.2003.04026.x. PMID 12603397. S2CID 8639102.




